- Overview
-
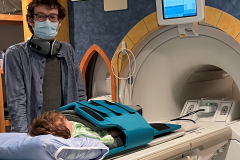
I am interested in the development of new tools that will help us detect lung disease in children. Specifically, this includes new, more sensitive breathing tests that will help us measure lung function in children. As well, I am interested in developing new imaging tests (such as MRI) that will help us see the structure of the lung.
My research focuses primarily, but not exclusively, on patients with cystic fibrosis.
- Publications
-
Heterogeneity of short-term elexacaftor-tezacaftor-ivacaftor response in cystic fibrosis using 129Xe MRI
Thorax
Rachel L Eddy and Vanessa M Diamond and Josie Chrenek and Girija Bhatnagar and David Sag and Rana Ghadymimahani and Amreen Aulakh and Britney X Ha and Bradley S Quon and Jonathan H Rayment
DOI: 10.1136/thorax-2025-223687
12/2025Home Microbiological Sampling in a Pediatric Cystic Fibrosis Population: Pandemic Implementation and Ongoing Use
Pediatric Pulmonology
Valerie Swanston and Jeffrey N. Bone and Melissa Richmond and David Goldfarb and Jonathan H. Rayment
DOI: 10.1002/ppul.71378
11/2025Utility of Hyperpolarized 129-Xenon MRI in Primary Ciliary Dyskinesia
ERJ Open Research
Wallace B. Wee and Brandon Zanette and Samal Munidasa and Rachel L. Eddy and Jonathan H Rayment and Teresa To and Felix Ratjen and Giles Santyr and Sharon D. Dell
DOI: 10.1183/23120541.01105-2025
10/2025Monitoring for paediatric pulmonary graft versus host disease with multiple breath washout
ERJ Open Research
Britney X. Ha and Juliana P. Roden and Rodrigo A. Sandoval and Kirk R. Schultz and Jonathan H. Rayment
DOI: 10.1183/23120541.00015-2025
09/2025The Canadian Lung Outcomes in Users of Vaping Devices (CLOUD) Study: Protocol for a prospective, observational cohort study
BMJ Open
Burns, P. and Eddy, R.L. and Li, X. and Yang, J. and Dhillon, S.S. and Couillard, S. and Stickland, M.K. and Guenette, J. and Svenningsen, S. and Tulloch, T. and Samji, H. and Meza, R. and Struik, L.L. and Aaron, S. and Ho, T. and Lam, S. and Leipsic, J. and MacLean, J. and Afshar, T. and Moraes, T.J. and Zanette, B. and Santyr, G. and Counil, F.-P. and Hernandez Cordero, A.I. and Matano, S. and De Arruda Maluf, G. and Leung, C. and Feng, C. and Bal, L. and Dhaliwal, H. and Mumuni, A. and Lui, C. and Drew, H. and Sin, D.D. and Rayment, J.H. and Leung, J.M.
DOI: 10.1136/bmjopen-2025-100568
2025Repeatability of Multiple Breath Washout in Pediatric Primary Ciliary Dyskinesia
Pediatric Pulmonology
Wee, W.B. and Bashi, L.M. and Jensen, R. and Rayment, J.H. and To, T. and Ratjen, F. and Santyr, G. and Dell, S.D.
DOI: 10.1002/ppul.71107
2025Pulmonary 129Xe MRI: CNN Registration and Segmentation to Generate Ventilation Defect Percent with Multi-center Validation
Academic Radiology
Mozaffaripour, A. and Matheson, A.M. and Rahman, O. and Sharma, M. and Kooner, H.K. and McIntosh, M.J. and Rayment, J. and Eddy, R.L. and Svenningsen, S. and Parraga, G.
DOI: 10.1016/j.acra.2024.10.029
2025Hyperpolarized129XE MRI and Spectroscopy: Quantitative Measurements, Results, and Emerging Opportunities
Radiology Cardiothoracic Imaging
Schmidt, A. and Liggins, J.A. and Bhutta, H. and Dell, S.D. and Leung, J.M. and Sin, D.D. and Leipsic, J.A. and Rayment, J.H. and Eddy, R.L.
DOI: 10.1148/ryct.240562
2025A multimorphic variant in ThPOK causes an inborn error of immunity with T cell defects and fibrosis
Journal of Experimental Medicine
Vaseghi-Shanjani, M. and Sharma, M. and Yousefi, P. and Samra, S. and Laverty, K.U. and Jolma, A. and Razavi, R. and Yang, A.H.W. and Albu, M. and Golding, L. and Lee, A.F. and Tan, R. and Richmond, P.A. and Bosticardo, M. and Rayment, J.H. and Yang, C.L. and Hildebrand, K.J. and Brager, R. and Demos, M.K. and Lau, Y.-L. and Notarangelo, L.D. and Hughes, T.R. and Biggs, C.M. and Turvey, S.E.
DOI: 10.1084/jem.20241174
2025Three-Dimensional Free-Breathing Ultrashort Echo Time (UTE) 1H MRI Regional Ventilation: Comparison With Hyperpolarized 129Xe MRI and Pulmonary Function Testing in Healthy Volunteers and People With Cystic Fibrosis
NMR in Biomedicine
Tan, F. and Eddy, R. and Diamond, V. and Rayment, J. and Larson, P.
DOI: 10.1002/nbm.70033
2025Risk Factors for Severe Disease Among Children Hospitalized With Respiratory Syncytial Virus
JAMA Network Open
Kirolos, N. and Mtaweh, H. and Datta, R.R. and Farrar, D.S. and Seaton, C. and Bone, J.N. and Muttalib, F. and Kaziev, C.L. and Fortini, J. and Mahant, S. and Campigotto, A. and Freire, G. and Yeung, R.S.M. and Rayment, J.H. and Yang, C. and Srigley, J.A. and Sadarangani, M. and Buchanan, F. and Morris, S.K. and Gill, P.J.
DOI: 10.1001/jamanetworkopen.2025.4666
2025A Systematic Review of the Variability of Ventilation Defect Percent Generated From Hyperpolarized Noble Gas Pulmonary Magnetic Resonance Imaging
Journal of Magnetic Resonance Imaging
Diamond, V.M. and Bell, L.C. and Bone, J.N. and Driehuys, B. and Menchaca, M. and Santyr, G. and Svenningsen, S. and Thomen, R.P. and Marshall, H. and Smith, L.J. and Collier, G.J. and Wild, J.M. and Woods, J.C. and Fain, S.B. and Eddy, R.L. and Rayment, J.H.
DOI: 10.1002/jmri.29746
2025Maximising opportunity for therapeutic success: sequential participation in cystic fibrosis nucleic acid-based therapy trials
Lancet Respiratory Medicine
Mayer-Hamblett, N. and Kerper, N.R. and Clancy, J.P. and Davies, J.C. and Taylor-Cousar, J.L. and Donaldson, S.H. and Bell, S.C. and Jain, R. and Simmonds, N.J. and Mall, M.A. and Goss, C.H. and Rayment, J.H. and Setiawan, L. and Pilewski, J.M.
DOI: 10.1016/S2213-2600(25)00206-1
2025Long-Term Safety and Efficacy of Elexacaftor/Tezacaftor/Ivacaftor in Children >6 Years with Cystic Fibrosis and at Least One F508del Allele: A 192-Week, Phase 3, Open-Label Extension Study
American Journal of Respiratory and Critical Care Medicine
Wainwright, C. and McColley, S.A. and McNally, P. and Powers, M. and Ratjen, F. and Rayment, J.H. and Retsch-Bogart, G. and Roesch, E. and Ramsey, B. and McKone, E.F. and Tullis, E. and Mall, M.A. and Taylor-Cousar, J.L. and Waltz, D. and Ahluwalia, N. and Chu, C. and Scirica, C.V. and Davies, J.C.
DOI: 10.1164/rccm.202502-0512OC
2025Corrigendum to Diagnosis of post-hematopoietic stem cell transplant bronchiolitis obliterans syndrome in children: time for a rethink? Transplantation and Cellular Therapy. 2024 Aug;30(8):760-769 (Transplantation and Cellular Therapy (2024) 30(8) (760–769), (S2666636724004111), (10.1016/j.jtct.2024.05.012))
Transplantation and Cellular Therapy
Shanthikumar, S. and Gower, W.A. and Cooke, K.R. and Bergeron, A. and Schultz, K.R. and Barochia, A. and Tamae-Kakazu, M. and Charbek, E. and Reardon, E.E. and Calvo, C. and Casey, A. and Cheng, P.C. and Cole, T.S. and Davies, S.M. and Das, S. and De, A. and Deterding, R.R. and Liptzin, D.R. and Mechinaud, F. and Rayment, J.H. and Robinson, P.D. and Siddiah, R. and Stone, A. and Srinivasin, S. and Towe, C.T. and Yanik, G.A. and Iyer, N.P. and Goldfarb, S.B.
DOI: 10.1016/j.jtct.2025.05.009
2025A multimorphic variant in ThPOK causes a novel human disease characterized by T cell abnormalities, immunodysregulation, allergy, and fibrosis
medRxiv
Vaseghi-Shanjani, M. and Sharma, M. and Yousefi, P. and Samra, S. and Laverty, K.U. and Jolma, A. and Razavi, R. and Yang, A.H.W. and Albu, M. and Golding, L. and Lee, A.F. and Tan, R. and Richmond, P.A. and Bosticardo, M. and Rayment, J.H. and Yang, C.L. and Hildebrand, K.J. and Brager, R. and Demos, M.K. and Lau, Y.L. and Notarangelo, L.D. and Hughes, T.R. and Biggs, C.M. and Turvey, S.E.
DOI: 10.1101/2024.06.26.24309360
2024Diagnosis of Post-Hematopoietic Stem Cell Transplantation Bronchiolitis Obliterans Syndrome in Children: Time for a Rethink?
Transplantation and Cellular Therapy
Shanthikumar, S. and Gower, W.A. and Cooke, K.R. and Bergeron, A. and Schultz, K.R. and Barochia, A. and Tamae-Kakazu, M. and Charbek, E. and Reardon, E.E. and Calvo, C. and Casey, A. and Cheng, P.C. and Cole, T.S. and Davies, S.M. and Das, S. and De, A. and Deterding, R.R. and Liptzin, D.R. and Mechinaud, F. and Rayment, J.H. and Robinson, P.D. and Siddaiah, R. and Stone, A. and Srinivasin, S. and Towe, C.T. and Yanik, G.A. and Iyer, N.P. and Goldfarb, S.B.
DOI: 10.1016/j.jtct.2024.05.012
2024Detection of Bronchiolitis Obliterans Syndrome after Pediatric Hematopoietic Stem Cell Transplantation An Official American Thoracic Society Clinical Practice Guideline
American Journal of Respiratory and Critical Care Medicine
Shanthikumar, S. and Goldfarb, S. and Abts, M. and Barochia, A. and Bergeron, A. and Blinman, T. and Bracken, J. and Calvo, C. and Casey, A. and Charbek, E. and Cheng, P.C. and Cole, T.S. and Cooke, K.R. and Das, S. and Davies, S.M. and De, A. and Deterding, R.R. and Gower, W.A. and Gross, J. and Iyer, N.P. and Liptzin, D.R. and Mechinaud, F. and Rayment, J.H. and Reardon, E.E. and Robinson, P.D. and Schultz, K.R. and Sheshadri, A. and Siddaiah, R. and Srinivasan, S. and Stone, A. and Tamae-Kakazu, M. and Teusink-Cross, A. and Towe, C.T. and Walkup, L.L. and Yanik, G.A.
DOI: 10.1164/rccm.202406-1117ST
2024Frequent microbiological surveillance during inpatient cystic fibrosis pulmonary exacerbations has limited clinical value: Respiratory culture monitoring during exacerbation
Journal of Cystic Fibrosis
Song, W.H. and Wong, K.S. and Goldfarb, D.M. and Bone, J.N. and Rayment, J.H.
DOI: 10.1016/j.jcf.2023.10.007
2024Emergence of the natural history of Myhre syndrome: 47 patients evaluated in the Massachusetts General Hospital Myhre Syndrome Clinic (2016–2023)
American Journal of Medical Genetics, Part A
Lin, A.E. and Scimone, E.R. and Thom, R.P. and Balaguru, D. and Kinane, T.B. and Moschovis, P.P. and Cohen, M.S. and Tan, W. and Hague, C.D. and Dannheim, K. and Levitsky, L.L. and Lilly, E. and DiGiacomo, D.V. and Masse, K.M. and Kadzielski, S.M. and Zar-Kessler, C.A. and Ginns, L.C. and Neumeyer, A.M. and Colvin, M.K. and Elder, J.S. and Learn, C.P. and Mou, H. and Weagle, K.M. and Buch, K.A. and Butler, W.E. and Alhadid, K. and Musolino, P.L. and Sultana, S. and Bandyopadhyay, D. and Rapalino, O. and Peacock, Z.S. and Chou, E.L. and Heidary, G. and Dorfman, A.T. and Morris, S.A. and Bergin, J.D. and Rayment, J.H. and Schimmenti, L.A. and Lindsay, M.E.
DOI: 10.1002/ajmg.a.63638
2024A randomised trial of oral prednisone for cystic fibrosis pulmonary exacerbation treatment
European Respiratory Journal
Waters, V. and Shaw, M. and Perrem, L. and Quon, B.S. and Tullis, E. and Solomon, M. and Rayment, J.H. and Lavoie, A. and Tse, S.M. and Daigneault, P. and Bilodeau, L. and Price, A. and Nicholson, M. and Chin, M. and Parkins, M. and McKinney, M.L. and Tam, J.S. and Stanojevic, S. and Grasemann, H. and Ratjen, F.
DOI: 10.1183/13993003.02278-2023
2024Advancing the pipeline of cystic fibrosis clinical trials: a new roadmap with a global trial network perspective
The Lancet Respiratory Medicine
Mayer-Hamblett, N. and Clancy, J.P. and Jain, R. and Donaldson, S.H. and Fajac, I. and Goss, C.H. and Polineni, D. and Ratjen, F. and Quon, B.S. and Zemanick, E.T. and Bell, S.C. and Davies, J.C. and Jain, M. and Konstan, M.W. and Kerper, N.R. and LaRosa, T. and Mall, M.A. and McKone, E. and Pearson, K. and Pilewski, J.M. and Quittell, L. and Rayment, J.H. and Rowe, S.M. and Taylor-Cousar, J.L. and Retsch-Bogart, G. and Downey, D.G.
DOI: 10.1016/S2213-2600(23)00297-7
2023Multiple breath washout and oscillometry after allogenic HSCT: a scoping review
European Respiratory Review
Sonneveld, N. and Rayment, J.H. and Robinson, P.D. and Usemann, J. and Nielsen, K.G.
DOI: 10.1183/16000617.0251-2022
2023Long-Term Safety and Efficacy of Elexacaftor/Tezacaftor/Ivacaftor in Children Aged >6 Years with Cystic Fibrosis and at Least One F508del Allele A Phase 3, Open-Label Clinical Trial
American Journal of Respiratory and Critical Care Medicine
Wainwright, C. and McColley, S.A. and McNally, P. and Powers, M. and Ratjen, F. and Rayment, J.H. and Retsch-Bogart, G. and Roesch, E. and Ahluwalia, N. and Chin, A. and Chu, C. and Lu, M. and Menon, P. and Waltz, D. and Weinstock, T. and Zelazoski, L. and Davies, J.C.
DOI: 10.1164/rccm.202301-0021OC
2023Genetics of bronchopulmonary dysplasia: An update
Seminars in Perinatology
Lavoie, P.M. and Rayment, J.H.
DOI: 10.1016/j.semperi.2023.151811
2023Phase 3 Open-Label Clinical Trial of Elexacaftor/Tezacaftor/Ivacaftor in Children Aged 2–5 Years with Cystic Fibrosis and at Least One F508del Allele
American Journal of Respiratory and Critical Care Medicine
Goralski, J.L. and Hoppe, J.E. and Mall, M.A. and McColley, S.A. and McKone, E. and Ramsey, B. and Rayment, J.H. and Robinson, P. and Stehling, F. and Taylor-Cousar, J.L. and Tullis, E. and Ahluwalia, N. and Chin, A. and Chu, C. and Lu, M. and Niu, T. and Weinstock, T. and Ratjen, F. and Rosenfeld, M.
DOI: 10.1164/rccm.202301-0084OC
2023Heterogenous Disease Course and Long-Term Outcome of Children’s Interstitial Lung Disease Related to Filamin A Gene Variants
Annals of the American Thoracic Society
Julia Carlens and K. Taneille Johnson and Andrew Bush and Diane Renz and Ute Hehr and Florian Laenger and Claire Hogg and Martin Wetzke and Nicolaus Schwerk and Jonathan H. Rayment
DOI: 10.1513/AnnalsATS.202202-142OC
12/2022A Phase 3, Open-Label Study of Lumacaftor/Ivacaftor in Children 1 to Less Than 2 Years of Age with Cystic Fibrosis Homozygous for F508del-CFTR
American Journal of Respiratory and Critical Care Medicine
Jonathan H. Rayment and Fadi Asfour and Margaret Rosenfeld and Mark Higgins and Lingyun Liu and Molly Mascia and Hildegarde Paz-Diaz and Simon Tian and Rachel Zahigian and Susanna A. McColley
DOI: 10.1164/rccm.202204-0734OC
11/2022CFTR modulators increase risk of acute pancreatitis in pancreatic insufficient patients with cystic fibrosis
Journal of Cystic Fibrosis
Michelle J. Gould and Haley Smith and Jonathan H Rayment and Helen Machida and Tanja Gonska and Gary J. Galante
DOI: 10.1016/j.jcf.2021.09.010
07/2022Multiple Breath Washout Testing to Identify Pulmonary Chronic Graft Versus Host Disease in Children After Hematopoietic Stem Cell Transplantation
Transplantation and Cellular Therapy
Jonathan H. Rayment and Rodrigo A. Sandoval and Juliana P. Roden and Kirk R. Schultz
DOI: 10.1016/j.jtct.2022.02.002
06/2022Pulmonary functional MRI: Detecting the structure–function pathologies that drive asthma symptoms and quality of life
Respirology
Kooner, H.K. and McIntosh, M.J. and Desaigoudar, V. and Rayment, J.H. and Eddy, R.L. and Driehuys, B. and Parraga, G.
DOI: 10.1111/resp.14197
2022All hands on deck: A multidisciplinary approach to SARS-CoV-2-associated MIS-C
Paediatrics and Child Health (Canada)
Lopez, A.A. and Patel, M. and Rayment, J.H. and Tam, H. and Roberts, A. and Laskin, S. and Tucker, L. and Biggs, C.M. and Ahmed, M.A. and Barakauskas, V. and Galanis, E. and Goldfarb, D. and Halparin, J. and Harris, K.C. and Kissoon, N. and Lawrence, S. and McGuffin, D. and Meckler, G. and Noel, K. and Schrader, D. and Sherwood, M. and Singh, A. and Vercauteren, S.
DOI: 10.1093/pch/pxab110
2022The effect of inhaled hypertonic saline on lung structure in children aged 3–6 years with cystic fibrosis (SHIP-CT): a multicentre, randomised, double-blind, controlled trial
The Lancet Respiratory Medicine
Tiddens, H.A.W.M. and Chen, Y. and Andrinopoulou, E.-R. and Davis, S.D. and Rosenfeld, M. and Ratjen, F. and Kronmal, R.A. and Hinckley Stukovsky, K.D. and Dasiewicz, A. and Stick, S.M. and Anthony, M.M. and Au, J. and Belessis, Y. and Bonte, M. and Cheney, J. and Clem, C. and Clements, B. and Cooper, P. and Davis, S.D. and Davis, M. and de Boeck, K. and de Marchis, M. and De Wachter, E. and Delaisi, B. and Delaup, V. and DeRicco, A. and Foti, A. and Gan, R. and Garriga, L. and Gartner, S. and Genatossio, A. and Grogan, S. and Hilton, J. and Hoppe, J.E. and Janssens, H.M. and Jensen, R. and Johnson, R. and Kemner-van de Corput, M.P.C. and Klein, B. and Kronmal, R.A. and Lucca, F. and Lucidi, V. and Montemitro, E. and Nahidi, L. and Nielsen, K.G. and Pearce, K. and Pittman, J.E. and Powers, M. and Prentice, C. and Pressler, T. and Rayment, J.H. and Reix, P. and Retsch-Bogart, G. and Riera, L. and Robinson, P. and Robinson, P. and Sanders, D.B. and Sandoval, R.A. and Sandvik, R.M. and Saunders, C. and Siegel, M. and Smith, J. and Solomon, M. and Stanojevic, S. and Tai, A. and Tiddens, H.A.W.M. and van de Puttelaar, J. and Van den Brande, C. and van Straten, M. and Vermeulen, F. and Volpi, S. and Wainwright, C.E. and Weiner, D.J. and Yuan, Y. and Zaimeddine, S.
DOI: 10.1016/S2213-2600(21)00546-4
2022All hands on deck: A multidisciplinary approach to SARS-CoV-2-associated MIS-C,Tout le monde sur le pont: une approche multidisciplinaire du SRAS-CoV-2 associe au SIME
Paediatrics and Child Health (Canada)
Lopez, A.A. and Patel, M. and Rayment, J.H. and Tam, H. and Roberts, A. and Laskin, S. and Ahmed, M.A. and Barakauskas, V. and Galanis, E. and Goldfarb, D. and Halparin, J. and Harris, K.C. and Kissoon, N. and Lawrence, S. and Mcguffin, D. and Meckler, G. and Noel, K. and Schrader, D. and Sherwood, M. and Singh, A. and Vercauteren, S. and Tucker, L. and Biggs, C.M.
DOI: 10.1093/pch/pxac018
2022Diffuse alveolar haemorrhage in a child with trisomy 21
Journal of Paediatrics and Child Health
Susan Telencoe and Ajay C Kevat and Anna F Lee and Jonathan H Rayment
DOI: 10.1111/jpc.15331
10/2021A phase 3 open-label study of elexacaftor/tezacaftor/ivacaftor in children 6 through 11 years of age with cystic fibrosis and at least one F508del allele
American Journal of Respiratory and Critical Care Medicine
Zemanick, E.T. and Taylor-Cousar, J.L. and Davies, J. and Gibson, R.L. and Mall, M.A. and McKone, E.F. and McNally, P. and Ramsey, B.W. and Rayment, J.H. and Rowe, S.M. and Tullis, E. and Ahluwalia, N. and Chu, C. and Ho, T. and Moskowitz, S.M. and Noel, S. and Tian, S. and Waltz, D. and Weinstock, T.G. and Xuan, F. and Wainwright, C.E. and McColley, S.A.
DOI: 10.1164/rccm.202102-0509OC
2021Protocols for multi-site trials using hyperpolarized 129Xe MRI for imaging of ventilation, alveolar-airspace size, and gas exchange: A position paper from the 129Xe MRI clinical trials consortium
Magnetic Resonance in Medicine
Niedbalski, P.J. and Hall, C.S. and Castro, M. and Eddy, R.L. and Rayment, J.H. and Svenningsen, S. and Parraga, G. and Zanette, B. and Santyr, G.E. and Thomen, R.P. and Stewart, N.J. and Collier, G.J. and Chan, H.-F. and Wild, J.M. and Fain, S.B. and Miller, G.W. and Mata, J.F. and Mugler, J.P. and Driehuys, B. and Willmering, M.M. and Cleveland, Z.I. and Woods, J.C.
DOI: 10.1002/mrm.28985
2021Comparison of Functional Free-Breathing Pulmonary 1H and Hyperpolarized 129Xe Magnetic Resonance Imaging in Pediatric Cystic Fibrosis
Academic Radiology
Couch, M.J. and Munidasa, S. and Rayment, J.H. and Voskrebenzev, A. and Seethamraju, R.T. and Vogel-Claussen, J. and Ratjen, F. and Santyr, G.
DOI: 10.1016/j.acra.2020.05.008
2021Free-breathing MRI for Monitoring Ventilation Changes following Antibiotic Treatment of Pulmonary Exacerbations in Pediatric Cystic Fibrosis.
The European respiratory journal
Munidasa S and Couch MJ and Rayment JH and Voskrebenzev A and Seethamraju R and Vogel-Claussen J and Ratjen F and Santyr G
DOI: 10.1183/13993003.03104-2020
PubMed: 33303537
12/2020Editorial for "Flow Volume Loop and Regional Ventilation Assessment Using Phase Resolved Functional Lung (PREFUL) MRI: Comparison With 129Xenon Ventilation MRI and Lung Function Testing".
Journal of magnetic resonance imaging : JMRI
Eddy RL and Rayment JH
DOI: 10.1002/jmri.27462
PubMed: 33314368
12/2020Factors influencing clinical trial participation for adult and pediatric patients with cystic fibrosis.
Journal of cystic fibrosis : official journal of the European Cystic Fibrosis Society
Lee M and Hu XY and Desai S and Kwong E and Fu J and Flores E and Lazosky L and Wilcox PG and Mcllwaine M and Chilvers M and Yang C and Rayment JH and Quon BS
DOI: 10.1016/j.jcf.2020.08.019
PubMed: 32900673
09/2020Sustained recovery of exocrine pancreatic function in a teenager with cystic fibrosis treated with ivacaftor
Pediatric Pulmonology
Smith, H. and Rayment, J.H.
DOI: 10.1002/ppul.24952
2020Assessing the feasibility of hyperpolarized 129Xe multiple-breath washout MRI in pediatric cystic fibrosis
Magnetic Resonance in Medicine
Couch, M.J. and Morgado, F. and Kanhere, N. and Kowalik, K. and Rayment, J.H. and Ratjen, F. and Santyr, G.
DOI: 10.1002/mrm.28099
2020Prolidase deficiency diagnosed by whole exome sequencing in a child with pulmonary capillaritis
ERJ Open Research
DOI: 10.1183/23120541.00205-2018
04/2019Hyperpolarised 129Xe magnetic resonance imaging to monitor treatment response in children with cystic fibrosis
European Respiratory Journal
Rayment, J.H. and Couch, M.J. and McDonald, N. and Kanhere, N. and Manson, D. and Santyr, G. and Ratjen, F.
DOI: 10.1183/13993003.02188-2018
2019Hyperpolarized Gas Magnetic Resonance Imaging of Pediatric Cystic Fibrosis Lung Disease
Academic Radiology
Santyr, G. and Kanhere, N. and Morgado, F. and Rayment, J.H. and Ratjen, F. and Couch, M.J.
DOI: 10.1016/j.acra.2018.04.024
2019An investigation into biomarkers for the diagnosis of ABPA and aspergillus disease in cystic fibrosis
Pediatric Pulmonology
Keown, K. and Abbott, S. and Kuzeljevic, B. and Rayment, J.H. and Chilvers, M.A. and Yang, C.L.
DOI: 10.1002/ppul.24465
2019Reply to Verbanck and Vanderhelst
American Journal of Respiratory and Critical Care Medicine
Kanhere, N. and Couch, M.J. and Rayment, J.H. and Ratjen, F. and Santyr, G.
DOI: 10.1164/rccm.201707-1392LE
2018The lung clearance index as a monitoring tool in cystic fibrosis: Ready for the clinic?
Current Opinion in Pulmonary Medicine
Perrem, L. and Rayment, J.H. and Ratjen, F.
DOI: 10.1097/MCP.0000000000000515
2018Lung clearance index to monitor treatment response in pulmonary exacerbations in preschool children with cystic fibrosis
Thorax
Rayment, J.H. and Stanojevic, S. and Davis, S.D. and Retsch-Bogart, G. and Ratjen, F.
DOI: 10.1136/thoraxjnl-2017-210979
2018Back to the source – Modern insights into pulmonary exacerbations and lung function decline from CF registry data
Journal of Cystic Fibrosis
Rayment, J.H. and Quon, B.S.
DOI: 10.1016/j.jcf.2018.05.001
2018Correcting for tissue nitrogen excretion in multiple breath washout measurements
PLoS ONE
Kane, M. and Rayment, J.H. and Jensen, R. and McDonald, R. and Stanojevic, S. and Ratjen, F.
DOI: 10.1371/journal.pone.0185553
2017Concomitant diffuse alveolar hemorrhage and pulmonary embolism in a child with isolated pulmonary capillaritis
Annals of the American Thoracic Society
Rayment, J.H. and Cutz, E. and Levy, D.M. and Dell, S.D.
DOI: 10.1513/AnnalsATS.201610-783LE
2017Chronic Hypoxemia in a 2-Year-Old Boy
Annals of the American Thoracic Society
Rayment, J.H. and Ahmareen, O. and John, P.R. and Ratjen, F.
DOI: 10.1513/AnnalsATS.201701-069CC
2017Another brick in the wall: Lung clearance index and lower airways pathology in preschool cystic fibrosis
Annals of the American Thoracic Society
Rayment, J.H. and Ratjen, F.
DOI: 10.1513/AnnalsATS.201706-432ED
2017Correlation of lung clearance index with hyperpolarized 129xe magnetic resonance imaging in pediatric subjects with cystic fibrosis
American Journal of Respiratory and Critical Care Medicine
Kanhere, N. and Couch, M.J. and Kowalik, K. and Zanette, B. and Rayment, J.H. and Manson, D. and Subbarao, P. and Ratjen, F. and Santyr, G.
DOI: 10.1164/rccm.201611-2228LE
2017Pulmonary Aspergillosis in a Previously Healthy 13-Year-Old Boy
Canadian Respiratory Journal
Rayment, J.H. and Narang, I.
DOI: 10.1155/2016/4575942
2016Culture-positive pediatric tuberculosis in Toronto, Ontario
Pediatric Infectious Disease Journal
Rayment, J.H. and Guthrie, J.L. and Lam, K. and Whelan, M. and Lee, B. and Jamieson, F.B. and Kitai, I.
DOI: 10.1097/INF.0000000000000915
2016Constrictive bronchiolitis: A distinct phenotype of cystic fibrosis lung disease?
Annals of the American Thoracic Society
Rayment, J.H. and Ratjen, F.
DOI: 10.1513/AnnalsATS.201609-701ED
2016ATS core curriculum 2016: Part III. Pediatric pulmonary medicine
Annals of the American Thoracic Society
Boyer, D. and Thomson, C.C. and Cohen, R. and Rao, D. and Dell, S. and Rayment, J. and Wang, R. and Dy, F.J. and Wambach, J. and Tam-Williams, J. and Simon, D. and Price, E. and Oermann, C.M. and Singh, A. and Rettig, J.S. and Duncan, E.D. and Baker, C.D. and Liptzin, D.R. and Moore, P.E.
DOI: 10.1513/AnnalsATS.201602-097CME
2016An unusual cause of empyema in a teenage boy
CMAJ
Rayment, J.H. and Weinstein, M.
DOI: 10.1503/cmaj.122089
2013Impact of the sentinel node frozen section result on the probability of additional nodal metastases as predicted by the MSKCC nomogram in breast cancer
Japanese Journal of Clinical Oncology
Jamal, M.H. and Rayment, J.H. and Meguerditchian, A. and Doi, S.A.R. and Meterissian, S.
DOI: 10.1093/jjco/hyq225
2011Integrin-linked kinase has a critical role in ErbB2 mammary tumor progression: Implications for human breast cancer
Oncogene
Pontier, S.M. and Huck, L. and White, D.E. and Rayment, J. and Sanguin-Gendreau, V. and Hennessy, B. and Zuo, D. and St-Arnaud, R. and Mills, G.B. and Dedhar, S. and Marshall, C.J. and Muller, W.J.
DOI: 10.1038/onc.2010.86
2010Addressing the role of cell adhesion in tumor cell dormancy
Cell Cycle
White, D.E. and Rayment, J.H. and Muller, W.J.
DOI: 10.4161/cc.5.16.2993
2006Amino acids as placeholders: Base-composition pressures on protein length in malaria parasites and prokaryotes
Applied Bioinformatics
Rayment, J.H. and Forsdyke, D.R.
DOI: 10.2165/00822942-200504020-00005
2005 - Research
-
Current Projects
Due to the remarkable advances in the care of children with cystic fibrosis (CF) over the past 3 decades, the traditional pulmonary function tests in most paediatric CF patients are normal. Despite this, we know that there is structural damage, inflammation and infection in the lungs of these children from an early age. In addition, new medical therapies for CF are leading to a monumental shift in how this disease is treated -- but again, if traditional pulmonary function testing is "normal" at the onset of therapy, it will not be sufficient to monitor response to treatment. For these reasons, new markers of lung health and disease are needed in this population. My research interests focus on the development of two types or pulmonary biomarkers: pulmonary function and imaging.
Multiple breath washout (MBW) testing is an old technique that has re-emerged in the literature over the past decade because it is extremely sensitive to the small airways disease that we see in early CF lung disease. There is, however, much that we don't know about this testing modality: how can/should it be used in a clinical setting? What constitutes a significant change between visits? Should a significant change in MBW outcomes prompt a change in clinical management? Through industry-initiated clinical trials and investigator-initiated studies, we hope to address these questions about this exciting new test.
Magnetic responance imaging is traditionally ineffective for imaging lung tissues, to its low proton density and high number of air/tissue interfaces. Novel techniques such as ultrashort echo time (UTE) MRI are improving the spatial resolution of pulmonary MRI, and are now being tested in children with CF. In addition, gas contrast imaging of the lungs using inhaled hyperpolarized noble gases (helium or xenon) allows for functional imaging. In collaboration with partners at UBC and St Paul's Hospital, I hope to develop a pediatric lung imaging research group at BCCH to use these emerging technologies in the investigation and care of children with lung disease.GrantsCF Canada Clinical Fellowship 2016-17
Honours & Awards2017 North American Cystic Fibrosis Conference Junior Clinical Investigator of the Year
Research Group MembersAmreen Aulakh, Undergraduate Student Research Assistant
Aysha Ayub, FLEX Student
Ernest Hoptioncann, Graduate Student
Jennifer Kwan, Research Ethics and Compliance Coordinator
Sabine Laguë, Graduate Research Assistant, Postdoctoral Fellow, Pediatric Respirology Fellow
Nicole Lee-Son, Physiotherapist - Researcher
Reece Long, FLEX Research Trainee
Alireza Mojibian, Research Manager, Program Manager - Pediatric Respiratory Research Team
Semipe Oni, Resident
Valerie Swanston, Medical Student Researcher
Helping kids with Cystic Fibrosis breathe easier: Q&A with new investigator Dr. Jonathan Rayment
As both a researcher and a doctor caring for patients, Dr. Jonathan Rayment is working to develop more sensitive and accurate tests of lung function in children. This could help doctors monitor children with CF and other lung conditions and provide them with treatment earlier, when it’s most effective.