COVID-19 research at BCCHR
(This page was last updated November 2, 2022)
As we enter our third year of the pandemic, it’s difficult to think of a time when COVID-19 did not dominate our lives.
The first reported case of COVID-19 in B.C. was on Jan 28, 2020, and at the time we were still scrambling to understand the implications of this brand new disease. We have learned a great deal since then and researchers at BC Children’s Hospital have greatly contributed to our understanding of the virus and helped find better ways to diagnose and treat COVID-19.
More than 80 studies related to COVID-19 have been initiated by BC Children’s researchers since the beginning of the pandemic, and the number keeps growing. Importantly, this research has occurred alongside the BC Children's Hospital Research Institute's (BCCHR) ongoing work on childhood diseases, child and family health, brain development and improving care through evidence and innovation.
This public health crisis reminds us, more than ever, of the importance of research in improving and transforming the mental and physical health of our children, families and communities.
Further research into the societal impact of the pandemic, long-term effects of the disease, and improved treatments and vaccines for SARS-CoV-2 will likely continue, and these pages will be updated to reflect this.
What is COVID-19?
COVID-19 is the name of the disease that occurs when someone is infected with severe acute respiratory syndrome coronavirus 2 virus (SARS-CoV-2). SARS-CoV-2 is a type of coronavirus, a family of viruses named for their crown-like shape when viewed under a microscope (corona is Latin for ‘crown’). Other coronaviruses typically cause mild to moderate respiratory illness, but they can also cause more serious illness as we saw in the 2002 to 2004 SARS outbreak.
SARS-CoV-2 infects cells by using its spike protein, which sits on the outside of the virus. The spike protein can bind to a molecule on human cells called the angiotensin converting enzyme-2 (ACE2) receptor. ACE2 breaks down a protein called angiotensin II into smaller components, which in turn regulate blood pressure and help reduce organ damage from inflammation. When the virus binds to the ACE2 receptor, it not only gains entry into the cell, but can also disrupt this pathway, leading to greater inflammation in the tissue. The ACE2 receptor is found on a wide variety of cells and organs in the body including the lungs, heart, blood vessels, kidney and liver.
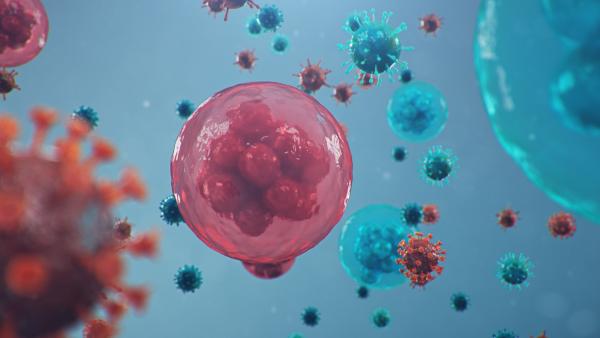
Once the virus is delivered into the cell, its single-stranded RNA (the coding instructions for making more of the virus) hijacks the cellular machinery to start making multiple copies of itself. These new copies are assembled and transported back out of the cell to infect others.
Thanks to researchers around the world concentrating their efforts on learning about SARS-CoV-2, the basic mechanics of the virus were uncovered early on. But many more questions arose.
How do we treat the virus and its symptoms? How can we best prevent transmission? How can we tell who is infected? What are the impacts on society? And later, once vaccines became available, how effective are they against infection and serious illness, and how are they best administered?
BC Children’s Hospital researchers have been at the forefront of the quest for new knowledge, impacting many aspects of how we diagnose and treat people, as well as public health decisions involving children, youth and families.