The Better Responses through Avatars and Evidence (BRAvE) Initiative at BC Children’s Hospital is revolutionizing precision treatments for children with cancer. The BRAvE team seeks to increase the number of children who can benefit from treatments targeted at attributes of individual tumours, battle hard-to-treat cancers, and reduce long-term health impacts. Generously supported by funding from BC Children’s Hospital Foundation and the Michael Cuccione Foundation, researchers at BC Children’s Hospital have developed a new precision oncology platform that stands to save young lives across Canada.
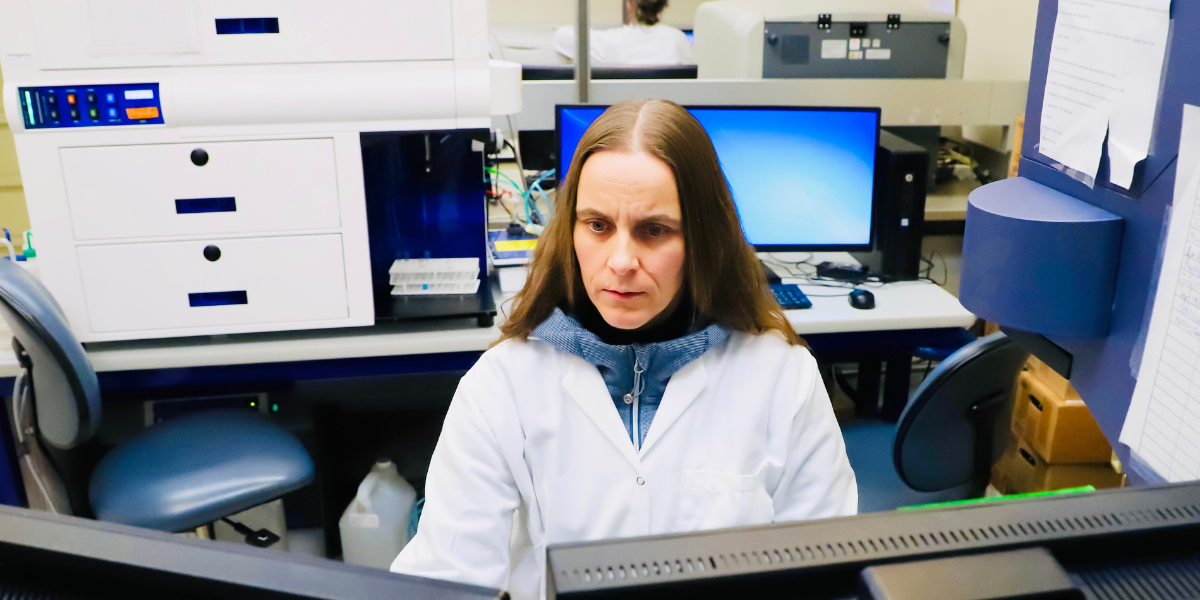
We recently sat down with Amanda Lorentzian and Dr. Nina Rolf to discuss their roles in the BRAvE Initiative and what makes BRAvE an exciting and unique precision medicine approach. Lorentzian is a PhD candidate co-supervised by Dr. Philipp Lange and Dr. Christopher Maxwell. Dr. Rolf is a physician-scientist and senior research associate who formerly completed a five-year postdoctoral fellowship under the supervision of Dr. Gregor Reid.

What are your roles within the BRAvE Initiative?
AL: I run the next-generation sequencing platform, which is what we use to detect DNA mutations in patients’ cancer cell samples from the BC Children's Hospital BioBank. I also use mass spectrometry to characterize all the proteins — or proteome — in the patients’ samples. My experiments focus on combining all of this information — from DNA and proteins — to better understand when pediatric cancers return or relapse, and how to best target each patient’s cancer.
NR: As a physician scientist, I am very involved in developing BRAvE. I did my clinical fellowship in pediatric hematology-oncology at BC Children’s Hospital and previously in Germany. I then completed a five-year postdoctoral fellowship with Dr. Gregor Reid in translational models for understanding pediatric leukemia. Now for BRAvE, I co-implement the research infrastructure or core technologies we use; analyze patient samples, determine how they are different from each other, and plan how we’ll xenograft them; and coordinate and oversee many aspects of BRAvE’s workflow. I also do a lot of single-cell analysis — in the context of leukemia and tumour immunology — to uncover the ways just a few cells can survive chemotherapy and drive a relapse later on.
How did you become involved in this work? Was it a natural next step in your education or career path, or did you deviate from what you were studying or working on before?
AL: It was a natural next step for me. Before beginning my research at BC Children’s Hospital Research Institute, I was working on cancer-related projects at a genomic sequencing company. I was happy with the work I was doing, but knew I wanted to be more involved in research. This led to my decision to pursue a PhD. The BRAvE Initiative felt like a perfect fit since I already had some experience with DNA sequencing and cancer, and the opportunity to learn more about proteomic and translational research was really exciting. Translational research is laboratory research that is meant to directly improve the care patients receive.
NR: In some ways it’s a deviation and in other ways it’s a natural progression. It’s a deviation because I’m a physician-scientist, but I’m currently not working clinically. And it’s a natural progression because I’ve long been interested in understanding why certain patients with leukemia relapse and how to figure that out before it happens as this is the key to a long-term cure for all. Additionally, I like investigating complex diseases from both clinical and scientific perspectives. I’m able to unite many of my interests and strengths in my work with the BRAvE Initiative.

What inspired you to work in the field of pediatric cancer?
AL: I really liked the idea of a comprehensive and individual approach and being able to use cutting-edge techniques to treat pediatric cancer. It’s inspiring to see many different labs and clinicians come together to work towards a common and very important goal.
NR: My clinical and research focus has been on leukemia, the most common pediatric cancer. We are able to cure more than 80 per cent of kids with the most common form of leukemia, acute lymphoblastic leukemia. However, in my work as a pediatric oncologist, it’s hard to see kids relapse because treatment options then are much more limited. It was so disheartening to me that relapsed leukemia has a very poor prognosis and that, even with the high initial cure rate, there are still too many kids who experience relapse. All of these factors inspired me to go into precision oncology and work on developing new diagnostic and treatment options.
What are you most excited to see happen as a result of the BRAvE Initiative?
AL: I think that even if one patient benefits from a treatment developed through BRAvE, that would be amazing and completely worthwhile! In five year’s time, ideally every patient with pediatric cancer will be enrolled in BRAvE from the time they’re first diagnosed. This is for two reasons. First of all, even children with a low risk of relapse still have a chance of their cancer coming back. If the molecular characterization performed by BRAvE is implemented early, then a personalized treatment option could be prepared and ready for them. And secondly, the more information and data we can collect, the better we can identify potential treatment targets, improve risk stratification, and determine better predictors of cancer relapse.
NR: We have seen some hopeful progress in the last five years, in that we have several novel treatment options to offer certain subsets of pediatric cancer patients. However, we still don’t fully understand why each patient’s cancer cells look and behave differently — even when they have been diagnosed with the same type of cancer. So I’m most curious about understanding what’s going on with each patient’s disease and figuring out the underlying factors and patterns. Therefore, I focus on delineating the relapse-driving components at the single-cell level in each patient, which is at the heart of developing precision medicine approaches. Ultimately, I want to see the BRAvE Initiative eliminate pediatric cancer recurrence. We aim to treat children so they survive and live healthy lives. We will not immediately cure cancer once and for all, but we will be able to identify more and more patients whose cancer will be cured more easily.
What do you most want BCCHR readers to know about the BRAvE Initiative?
AL: I want to express my gratitude to the patients and families that participate in BRAvE and BCCH BioBank studies. I would also like to thank the Michael Cuccione family for your ongoing support of our research and the BCCH Biobank for coordinating the studies and collecting the samples. You all make our work possible!
NR: The BRAvE Initiative is amazing. We are a multidisciplinary team able to look at one cell from multiple different angles and perspectives. Also, we work as a real team. We have so many discussions to finetune the questions we ask and integrate the answers and insights we generate. It’s an incredible honour to be part of the BRAvE Initiative. I am convinced that together we will make a real difference in curing more children with leukemia.




