 A new methodology developed by researchers at BC Children’s Hospital, the University of British Columbia and The Canadian National Transplant Research Program could speed the discovery of new biomarkers and, in doing so, improve diagnosis and care for kids who have immune-related diseases or have undergone a cell or tissue transplant.
A new methodology developed by researchers at BC Children’s Hospital, the University of British Columbia and The Canadian National Transplant Research Program could speed the discovery of new biomarkers and, in doing so, improve diagnosis and care for kids who have immune-related diseases or have undergone a cell or tissue transplant.
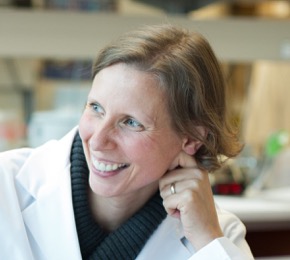
“Biomarkers give doctors a personalized and accurate insight into how a disease is progressing and whether treatment is working as expected,” says Dr. Megan Levings, an investigator at BC Children’s Hospital. “For kids with immune disorders, identifying new biomarkers means that doctors are better able to determine the right treatment. In the case of kids who have undergone transplantation, biomarkers could help doctors catch the earliest signs of transplant rejection, greatly improving their chances of avoiding serious health conditions like diabetes and heart disease.”
Biomarkers are any substance in the body – like blood cells – that can be measured to shed light on a patient’s health. Recently published in JCI Insight, this detailed, easy-to-replicate protocol promises to overcome the common hurdles researchers face in identifying and validating new biomarkers and using these discoveries to improve clinical care.
“We’re finding a wealth of potential biomarkers in the lab, but it takes a long time to gather enough patient data to find out whether they’re useful for doctors and the children in their care,” says Dr. Sabine Ivison, Project Manager in the Levings Lab and lead author on the publication. “So we set out to change that.”
In immune-related diseases, the most promising biomarkers are often proteins or cells in the blood. Today, researchers use a technology called flow cytometry to discover new biomarkers, but the way this technology is applied can be subjective and time consuming.
With flow cytometry, researchers can count and analyze cells and their components. First, they use the technology to mark specific proteins or molecular ‘flags’ on the surface of blood cells with fluorescent dyes, called fluorochromes. Then, the cells are run through the equipment where specially calibrated lasers detect these fluorochromes, allowing the machine to count the cells and group them by type.
The key challenge researchers face with flow cytometry is replicating these results. One of the reasons for this is that, when a cell is marked with fluorescent dye, its brightness can vary substantially depending on machine configuration, operator handling or the protocol used to attach the dye. As a result, researchers often have to judge by eye which cells to include in their analysis, which can make it difficult to replicate or validate their results. Additionally, recent technological advances in flow cytometry have meant that many more fluorochromes can be attached to the same cells and processed at the same time. While this makes flow cytometry a more powerful research tool, it also means that analyzing the resulting data is far more complex and difficult to decipher without the aid of automated solutions.
To overcome these challenges, Dr. Levings, Dr. Ivison and colleagues developed a protocol that describes how to collect samples and label cell markers using commercially-available products, and analyze the samples using a computer program designed by study co-authors Dr. Ryan Brinkman and Dr. Mehrnoush Malek to process the data more quickly and reproducibly. With this new method, it takes just a minute of computer time to process 25 samples, while the equivalent manual analysis requires 10–20 hours of an expert’s time, sparing researchers from labour-intensive and subjective manual data analysis.
“The subjective nature of how flow cytometry is currently used has created a major bottleneck preventing researchers from pooling patient data and limiting work to smaller, single-institution studies,” says Dr. Ivison. “Enabling researchers and clinicians to analyze results the same way, allows them to make apples-to-apples comparisons across multiple hospitals and labs and gather the data they need to come to robust conclusions about their findings.”
To test and validate the methodology, the researchers took blood samples from healthy patients and those receiving blood transplants and sent them to be analyzed in five different centres across Canada. The team found that by following their new protocol, each centre could distinguish healthy patients from transplant recipients and, furthermore, arrived at similar results despite using different flow cytometry machines. This demonstrated that their protocol could be used to rapidly replicate and validate biomarkers across multiple institutions while searching for signs of disease.
“Making it easier to launch larger national studies is especially important for kids since most immune-related childhood diseases are uncommon and spread out across the country,” says Dr. Levings. “A single hospital or research institute may only encounter a handful of cases for some of the rarer childhood diseases, making it difficult to know how to improve care. By comparing results and verifying new biomarkers across the country, we can find better ways to diagnose and treat these children.”
Dr. Levings is the research lead for Childhood Diseases at BC Children’s Hospital and a professor at the department of Surgery at the University of British Columbia.
Participating centres in the study include BC Children’s Hospital Research Institute, Terry Fox Laboratory, Alberta Transplant Institute, Hôpital Maisonneuve-Rosemont, Toronto General Research Institute and CancerCare Manitoba.
This research is supported by Canadian Institutes of Health Research through the Canadian National Transplant Research Program, the National Institute of Allergy and Infectious Diseases of the NIH, and the Natural Sciences and Engineering Research Council.
Read more:
Ivison, S., Malek, M., Garcia, R.V., Broady, R., Halpin, A., Richaud, M., Brant, R.F., Wang, S., Goupil, M., Guan, Q., Ashton, P., Warren, J., Rajab, A., Urschel, S., Kumar, D., Streitz, M., Sawitzki, B., Schlickeiser, S., Bijl, J.J., Wall, D.A., Delisle, J., West, L.J., Brinkman, R.R., and Levings, M.K. (2018). A standardized immune phenotyping and automated data analysis platform for multicenter biomarker studies. JCI Insight, 3(23): e121867.




