Lindsay Pallo and Raelyn Gallant know too well how wonderful it would be to cure, prevent, or at least improve treatment for diabetes.
Pallo was diagnosed with type 1 diabetes at age eight, Gallant at age 10.
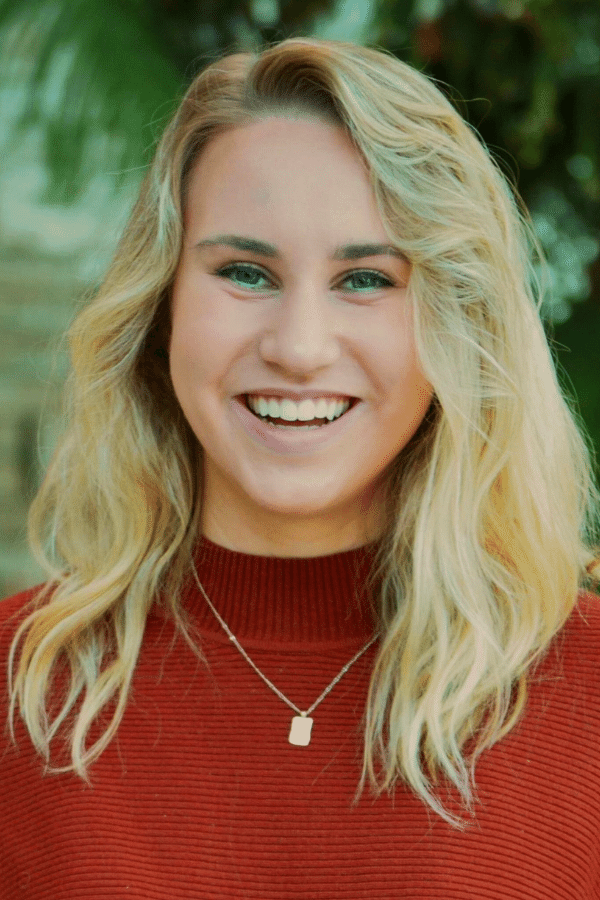
“I remember I used to get really hungry so I ate two-and-a-half foot-long subs,” Gallant says.
Type 1 diabetes develops when the immune system destroys insulin-producing beta cells in the pancreas, making individuals dependent on insulin injections for life. The chronic condition typically develops during childhood and affects an estimated 31,000 people in British Columbia.
Treatment involves managing the amount of glucose, or sugar, in the blood using insulin, diet and lifestyle to prevent complications, including heart disease, nerve, kidney, foot and eye damage.
In instances of T1D diabetes where blood glucose levels remain abnormally high, glucose from the blood cannot enter the cells so the body can’t convert food into energy — thus Gallant’s increased hunger.
Ninety per cent of Canadian adults with diabetes live with type 2 diabetes, a disease where the body does not produce enough insulin or doesn’t properly use the insulin their body makes. Type 2 diabetes is caused by risk factors that include high blood pressure, high cholesterol and a high body-mass index, some of which can be controlled, and some of which cannot.
The now 24-year-old Gallant calls type 1 diabetes a mental as well as a physical disease, noting that an invitation to grab a cookie and a coffee isn’t so straightforward. Someone with type 1 diabetes has to consider their blood sugars, how ingesting something will affect their blood glucose now and later, their forthcoming activities and how much stress they’re under.
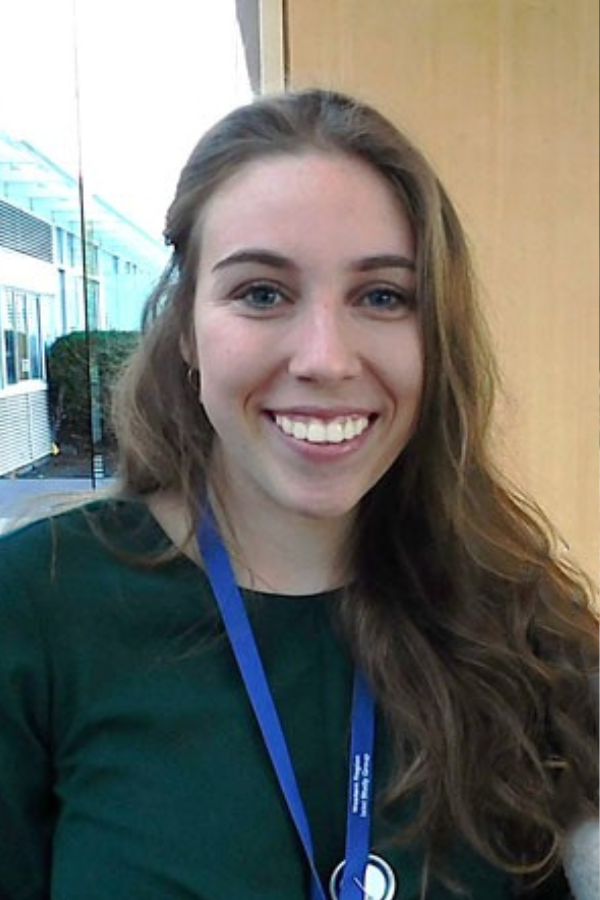
“It would be nice to not have to think about it all the time,” says the master’s student in Pathology and Laboratory Medicine at the University of British Columbia and a researcher in the lab of leading diabetes researcher Dr. Bruce Verchere.
“Even if you’re not sitting there concentrating on it, you’re always thinking about it in the back of your mind.”
The cost of supplies for monitoring and treating diabetes and keeping up with medical appointments can also be more stressful, adds Pallo.
“I remember last year I had to go to my annual eye doctor appointment and the ophthalmologist came in and said, ‘I think you’re the youngest one here by at least 40 years.’ It made me realize this isn’t something most young 20-years-olds have to do, keeping up with all the health appointments. I’m at risk for many, many side effects and other health complications in the future, which isn’t the nicest thing to think about,” says the 25-year-old doctoral student, also a researcher in Verchere’s lab.
Their research is personal
Pallo is working on two studies related to T1D.
In one study, she’s measuring the different proteins that beta cells release when they’re stressed to see if there’s a different level of beta cell dysfunction occurring that could indicate the imminent onset of type 1 diabetes. Such information could prove helpful for someone with T1D undergoing emerging treatments such as immunotherapy. Protein levels could be measured to determine how beta cells are responding to therapy, and therapy could be adjusted to bring those proteins to levels that reflect those in someone not living with T1D.
Pallo is also working on creating a drug delivery system to target immune cells and teach them not to attack beta cells in people who are at risk of developing type 1 diabetes.
Gallant is studying specialized cells called macrophages, or the “garbage eaters of the immune system,” to see whether they could be harnessed to help prevent both type 1 and type 2 diabetes from developing or, once it has developed, reverted.
Hopes for the future
Pallo hopes her research into treatments will ultimately release people with type 1 diabetes from the mental burden of living with the condition day-to-day.
“It’s too early to know whether this will be a one-and-done therapy, or something that people living with type 1 diabetes will need to take multiple times,” she says. “But anything to reduce the burden of having to check your blood glucose levels and take insulin several times every day, or needing to pack an extra suitcase just for your supplies if you go on vacation. It would be great if people could forget about their type 1 diabetes for longer than five minutes.”
“The best comparison I’ve heard is that living with type 1 diabetes is a full-time job on its own, and then you also have your actual full-time job on top of that. But you can never quit that first full-time job.”
For Gallant, her days in diabetes research are numbered. She ultimately aims to become a forensic pathologist, a physician who examines the corpses of people who’ve died suddenly.
“It’s hard to not sound like a maniac when I tell people that’s what I want to do,” she says with a laugh. “I grew up hunting, dissecting fish, dissecting deer. It was always a lot of fun poking different organs and seeing what they ate last, and doing autopsies is something I get excited about.”
Lived experience informing research
Both she and Pallo agree their lived experience enriches research because they are quick to ask how the findings will ultimately help people like them.
“More people who have personal connections to health research should consider entering the field,” Gallant says.
And you don’t have to be a researcher to contribute. Pallo notes people with lived experience can provide their expertise as patient partners.
“We’re including more patients in diabetes research who can provide their personal insights and experiences and show us what really matters to them in terms of how we communicate our science,” she says. “That’s such an important piece for researchers to consider.”




