
The Gut4Health team at BC Children's Hospital and the University of British Columbia is looking at new ways to target the gut microbiome to reduce inflammatory bowel disease (IBD) symptoms, increase treatment effectiveness and lead to long-term remission in pediatric IBD patients.
What is IBD?
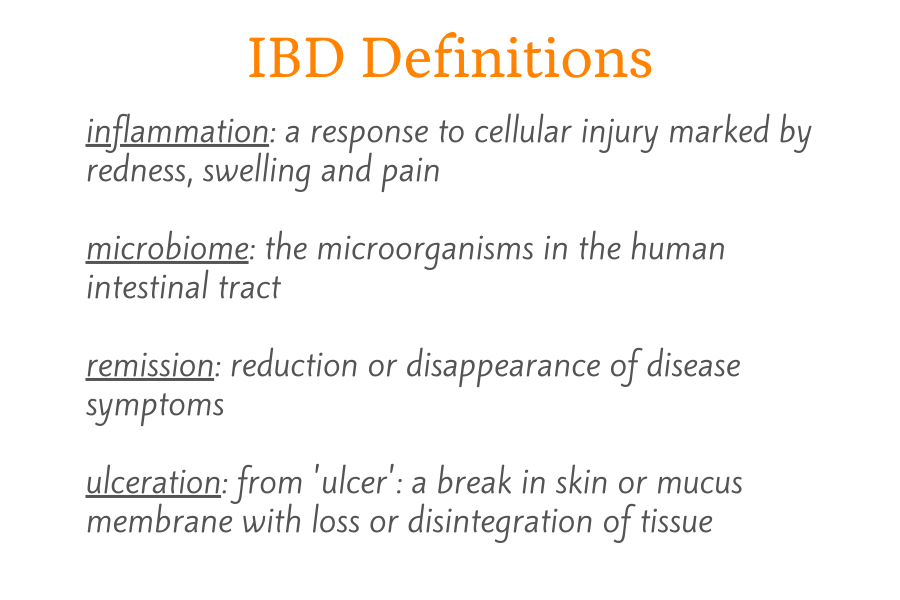
Inflammatory bowel disease is an umbrella term for a group of disorders that involve inflammation and ulceration of the gastrointestinal tract. Affecting both males and females, the main forms of IBD are Crohn's disease (CD) and ulcerative colitis (UC).
Symptoms of IBD can include diarrhea, fatigue, fever, weight loss and stomach pain. Over time, other areas of the body besides the digestive tract can become involved. Some individuals with IBD develop arthritis, skin disease, mouth sores, eye problems, osteoporosis (bone density loss), kidney stones, gallstones and additional complications.
Canadian children with IBD need new treatment options
Canada has among the highest rates of pediatric inflammatory bowel disease in the world. More than 7,000 Canadian children under the age of 18 have been diagnosed with IBD and around 650 Canadian children under 16 are newly diagnosed with the condition each year. The age group with the most rapidly rising incidence of IBD is children under five years old.
Inflammatory bowel disease is thought to be caused by complex interactions between genetics, the gut microbiome, and environmental factors — such as diet — that lead to an abnormal response by the immune system.
Individuals with IBD have a lower quality of life and increased risk of developing colorectal cancer when compared to the general population. While IBD treatments lead to remission for some individuals, treatment effectiveness is low for others. Combined with the challenges and risks associated with IBD therapies, such as adverse reactions to medication and psychological and social impacts, new treatments are in high demand.
The gold standard treatment for Crohn's disease is a liquid-only diet called exclusive enteral nutrition (EEN). EEN is typically administered for 1-3 months either by mouth or through a tube placed in the nose that delivers the EEN formula to the stomach.
While EEN does not cure CD in children, it promotes physical growth and mucosal healing, and can lead to temporary remission for many patients. Up to 30 per cent of CD patients do not respond to EEN, however, and the treatment does not usually help those with ulcerative colitis. Additionally, an imbalance of gut microorganisms called dysbiosis is associated with EEN. Dysbiosis may be a risk factor for developing other diseases and may ironically lead to future flare-ups (increase in symptoms) of IBD.
Gut4Health's first study: Developing a new exclusive enteral nutrition formula for IBD

Researchers with the Gut4Health team at BC Children's and UBC recently looked at using a new type of exclusive enteral nutrition formula in a mouse model of IBD. Specifically, they wanted to test whether adding a type of fibre called inulin-type fructans to EEN would increase the benefits of the treatment and lead to better overall disease outcomes.
"We suspect that the absence of certain prebiotics and fibre in EEN formula may be responsible for its reduced efficacy and outcomes in children with IBD," said Dr. Genelle Healey, first author of the team's research article published in Cellular and Molecular Gastroenterology and Hepatology.
"In our study, we hypothesized that the addition of inulin-type fructans would lead to beneficial changes in the gut microbiome and an increase in anti-inflammatory immune cells within the body," said Dr. Healey.
Inulin-type fructans can be classified as prebiotics since they beneficially alter the gut microbiome and improve human disease outcomes. Adding this prebiotic to EEN formula might aid in its use for ulcerative colitis patients and reduce the chance of developing microbial dysbiosis for both Crohn's and ulcerative colitis patients.
Inulin-type fructans and butyrate

"I chose inulin-type fructans for this study because of previous research showing its beneficial effects on the gut microbiome and butyrate production," said Dr. Healey.
Butyrate is a short-chain fatty acid produced through microbial fermentation of fibre in the intestinal tract and has been shown to protect against several diseases such as colorectal cancer, diabetes, obesity and IBD. Butyrate enhances the secretion of hormones that tell the brain that the stomach is full, helps maintain intestinal barrier function, improves insulin sensitivity and regulates important immune responses. Evidence suggests that butyrate helps dampen down inflammation and may have benefits in children who experience a worsening of their IBD.
The team's findings support their original hypothesis, providing an exciting and novel proof of concept. The inulin-enriched EEN group displayed a 100-fold increase in the abundance of a specific bacterium that produces butyrate along with a significant increase in butyrate concentrations. This group also showed greater protection against colitis, better gut microbiome balance, and higher survival rates compared to groups fed fibre-free EEN or regular chow.
The researchers propose that the mice fed inulin-enriched EEN were protected from developing colitis through a butyrate-dependent increase of anti-inflammatory regulatory T cells. These regulatory T cells, or Tregs, are immune cells that expand in the presence of high concentrations of butyrate and are essential in maintaining proper immune response.
Taking this research success to the bedside
"We are now planning a clinical study in children with ulcerative colitis and Crohn's disease, to compare the fibre-free versus the inulin-enriched EEN," said Dr. Healey.
The Gut4Health team hopes to collaborate with other researchers in Canada and other countries who have a similar interest in determining both the pro- and anti-inflammatory effects of different fibre types in inflammatory bowel disease.
"If we can completely prevent the dysbiosis that occurs with fibre-free EEN and maintain gut microbiome health, that may mean that our pediatric patients can stay in remission a lot longer," said Dr. Healey.

The research team is co-led by Dr. Bruce Vallance and Dr. Kevan Jacobson. In addition to Dr. Genelle Healey, the Vancouver team includes:
- Dr. Kevin Tsai
- Dr. Alana Schick
This research was supported by discovery grants from the Natural Sciences and Engineering Research Council, the Children with Intestinal and Liver Disorders (CH.I.L.D.) Foundation, operating grants from the Canadian Institutes of Health Research (CIHR), and Crohn's and Colitis Canada, and a Trainee Award from the Michael Smith Foundation for Health Research.
How can the Gut4Health core facility help you and your research team?
The primary goal of Gut4Health is to facilitate microbiome studies for researchers. Gut4Health is a centralized and cost-effective resource for processing and storing biological specimens as well as sequencing and analysis of microbial communities for various research studies, including basic science and clinical, translational and epidemiological projects.
To learn more about Gut4Health, check out Gut4Health Microbiome Core Facility.
Want to contact Gut4Health? Email Dr. Andy Sham, Project Manager, Gut4Health.




