
Globally, infectious diseases such as pneumonia and malaria are among the leading causes of death for children under five. Pneumonia alone claims the lives of more than 700,000 children under five annually, largely in low- and middle-income countries. A contributing factor is a shortage of essential health-care equipment and other resources for diagnosing and treating life-threatening cases of pediatric pneumonia in rural and under-resourced health-care centres.
Dr. Michael T. Hawkes, a new investigator at BC Children’s Hospital Research Institute (BCCHR), is working to change that by developing biomedical technologies and diagnostic tools to aid clinicians in triaging and treating the most severe cases of pneumonia. Dr. Hawkes, who is also an associate professor in the Faculty of Medicine at the University of British Columbia (UBC), specializes in pediatric infectious diseases such as pneumonia, malaria, HIV, and dengue fever. As a pediatric infectious diseases consultant at BC Children’s Hospital, he spends part of his time advising BC Children’s physicians on infectious diseases practices and antibiotic treatments for patients across the hospital. Dr. Hawkes, who is also a member of the Institute for Global Health at BC Children’s Hospital, is leading a research team in Uganda, which is where we reached him for a conversation about his work.
What initially brought you to pediatric medicine?
I started off in chemical engineering and switched to medicine because I was interested in biomedical applications of engineering. I was initially focused on biomedicine and scholarly research, but when I did my rotation in pediatrics, I just loved the children. I developed two main interests throughout medical school: one was tropical medicine and medicine in low-income settings, and the second was the children. Pediatric infectious diseases brings these two together in my research and as a clinician-scientist.
What led you to study pneumonia and other infectious diseases in resource-poor settings?
I am interested in global health and feel an ethical imperative to focus on the leading causes of death and disability in the world, not just diseases that affect Canadian children. I don’t think our responsibility stops at the border. I think there is a responsibility for wealthy countries like Canada to share our knowledge and resources, not as a neo-colonial approach to charity — but working hand-in-hand with people to solve these issues.
“I am interested in global health and feel an ethical imperative to focus on the leading causes of death and disability in the world.”
Can you tell us about your recent findings in Open Forum Infectious Diseases related to a finger-prick blood test for diagnosing pneumonia?
If a child comes to the hospital with a cough or difficulty breathing, you have to determine whether it’s a virus or bacteria and how severe it is. Depending on those answers, the child may need admission to the hospital, intravenous fluids, oxygen, and/or antibiotics. At the other end of the spectrum, they could be managed safely at home. At BC Children’s Hospital we can address those questions with a chest X-ray, but in low-resource settings that equipment is often not readily available.
In our recent study in Uganda, we demonstrated that a simple blood test may suffice to distinguish severity of pneumonia in children presenting with symptoms. We identified four different biomarkers that, together, were quite accurate in predicting those children with fluid in the lung, which is indicative of pneumonia. So instead of using an expensive chest X-ray machine, this blood test could be adapted to an affordable point-of-care tool similar to the COVID test. This could help in triaging the sickest children who need more resources for treatment.
You published a paper in The Lancet showing proof of concept for improved delivery of a pneumonia treatment in Uganda. What was the context, and what did you find?
I was in Uganda leading a trial for treatment of malaria when we realized we didn’t have enough oxygen for our patients. That was a finding from boots on the ground: practicing medicine in Uganda highlights gaps that you might not appreciate in Canada, where hospitals have ready access to oxygen. And it’s critical therapy for children with many diseases, including pneumonia, but in low-income settings, it’s not always available.
In Uganda, you have a couple of solutions. One is a pressurized oxygen cylinder, which works great but is a bit tricky to use and there are some safety issues. But the most important barrier for cylinders is stock management. In low-income settings, you’ll often find cylinders sitting empty because it’s expensive to transport them back and forth to the main city to refill them, due to the prohibitive cost of fuel.
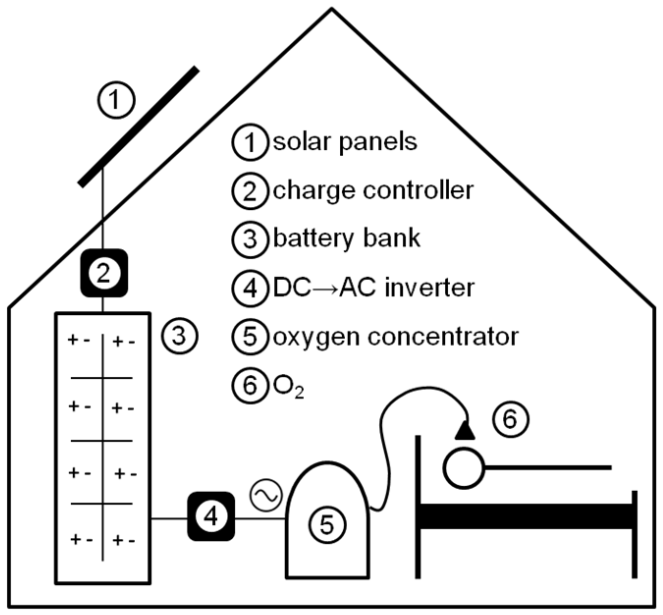
The second technology is concentrators — small machines that run on-site to extract and concentrate oxygen from room air for therapeutic use. They’re widely used in hospitals in Uganda, but their main limitation is power supply. There were incidents at Jinja Hospital where the power went out and children who were dependent on grid-powered concentrators died without their oxygen. So we came up with the solution of solar energy to power the concentrators. Using solar panels and a battery bank, the equipment can run 24/7 off the grid in the most rural areas.

In earlier studies, we established the viability and effectiveness of solar-powered oxygen concentration for treating pneumonia. Then, in a really exciting larger-scale trial with 20 sites and more than 2,400 children across Uganda (published in The Lancet in February), we showed that this technology reduced mortality by 49 per cent.
How can solar-powered O2 be scaled up? What are the next steps?
In the Solar Oxygen Study (SOS), we also showed cost-effectiveness. But the upfront cost of the equipment is much higher and not manageable for most under-resourced hospitals. So we’re currently pursuing solar-powered oxygen cylinder filling as a service. Rather than one solar-power system per hospital, we can fill a pressurized oxygen cylinder for far less than the full equipment setup. Doing this in more remote areas could get around the stock management issue. Imagine a hub-and-spoke model similar to bringing an empty barbecue propane tank to exchange for a full one. The hub is near the hospital, so you don’t have to pay for all that fuel to travel all the way to the capital city to fill your cylinder.
What else are you working on in Uganda right now and what are you planning to do in your work with BCCHR?
We’re setting up a lab here so we can do sample-processing and capacity-building with the Ugandans. Previously, we would run a study, collect and freeze the samples, and then ship them for analysis in Canada. This is fine, and there’s lots of expertise in Canada, but I think it’s better to develop local infrastructure and expertise among Ugandan lab staff. So we’re not just dropping in and collecting samples, we’re building local capacity.
“By practicing medicine in Uganda, you can see gaps that you might not appreciate in Canada.”
Another project I’m working on here in Uganda is called MALGUT, a study that’s funded through BCCHR. Together with Dr. David Goldfarb, a microbiologist and BCCHR investigator, our team is looking at malaria and the intestine. We’ll be observing bacteria in the stool of children with and without malaria and diarrhea to see if there is some interaction between the malaria parasite and the bacteria in the gut causing inflammation and leak. The gut may be a “motor of sepsis,” leading to severe outcomes in children with malaria. We’ll soon begin the study at Kambuga Hospital and use our brand new UBC lab to run the samples. That’s what’s exciting for me, that we can build infrastructure, and we’ll actually collect the data and samples and analyze many of them in-country.
What is it like working in Uganda and what is most interesting or rewarding about this work?
I try to come over here as much as possible because I quite like being here. I’m here for four weeks this time, and we’re in the early stages of the development of the UBC lab. I split my time between planning and meetings with the local Ugandan team, as well as planning our new MALGUT study. They also have an anthrax outbreak here currently, which is very interesting for an infectious diseases doctor. I have a license to practice medicine in Uganda, so I can help at the hospital, consulting on the children and on infectious diseases like anthrax. So I work both at our lab and at the hospital with patients.
I’m grateful to the BC Children’s Hospital Foundation, BCCHR, and UBC for the support which allows me to dedicate time to this field research in Uganda.




