Past Projects
Automatic detection of burst suppression patterns in EEG
Burst suppression (BS) is a measure commonly reported by EEG-based depth of hypnosis (DoH) monitors, used to warn the attending anaesthesiologist of over-sedation. The presence of suppression is generally considered detrimental to patient outcomes. Suppression is also an important marker for a number of serious clinical conditions. A problem with the existing BS detection algorithms is that they are fairly primitive, prone to false positive detection, and other incorrect readings, especially on vulnerable populations like the sick and elderly. Thus, developing an accurate automatic BS detection algorithm is important not only for the purpose of DoH monitoring during the surgery but also for improving ICU patient outcomes. In this work, we propose a systematic engineering effort to develop an improved BS detection algorithm that can be used as a replacement of current technology, contribute to the state of the art of EEG-based anesthesia monitoring, and be shared with the community.
High-Fidelity Data Converters for Medical Diagnostics
This project aims to develop a high-resolution analog-to-digital converter (ADC) optimized for biomedical signals, funded by Mitacs, in collaboration with industry partner ESS Technologies, which has expertise in audiophile-class microelectronics and interest in applying their technology to medical devices. The project consists of applying noise shaping control theory to produce a rigorous method of designing and analyzing a certain type of ADC. The converter of interest is the high-order sigma-delta modulator with single-bit quantization. This relatively simple architecture can have high signal-to-noise ratio, however, it is non-linear and requires techniques to maintain stability. Computer simulations of the proposed device will be run to optimize parameters. A physical field-programmable gate array (FPGA) prototype may be used to evaluate performance in digitizing biomedical signals.
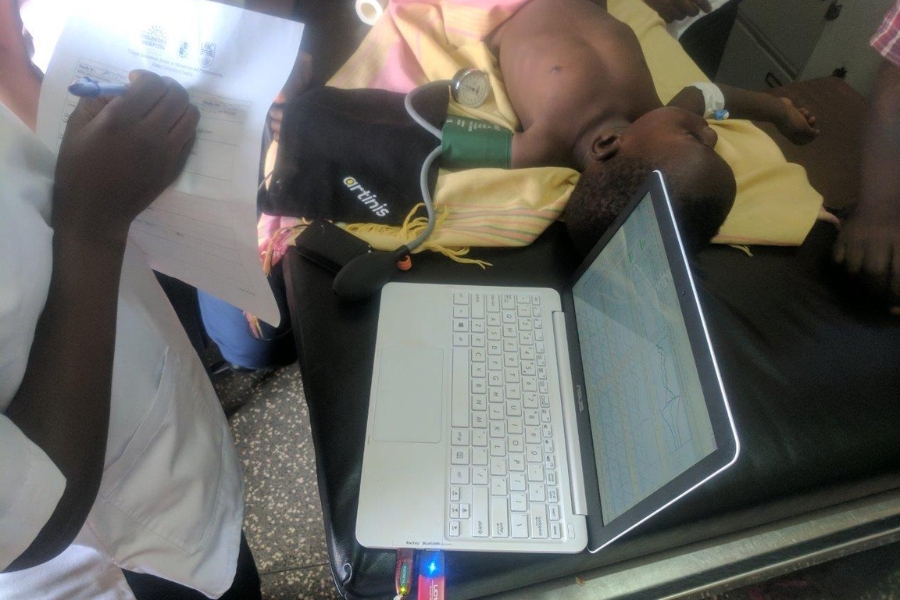
Tissue oxygen saturation in malnutrition and pneumonia
Founded by Grand Challenges Exploration, this study is one of our ongoing global health projects in Uganda, Africa. Children with moderate to severe malnutrition are more susceptible to get infections creating a vicious cycle of “infection-malnutrition”. Near Infrared Spectroscopy (NIRS) is a non-invasive technology which could be used in clinical settings to measure changes in tissue oxygenation and hemodynamics. The purpose of this study is to evaluate and develop a non-invasive diagnostic and treatment-progress monitoring tool to assess peripheral muscle oxygen saturation levels using NIRS. The absorption of very specific wavelengths of light in a child will provide an objective measure of a child’s metabolic status and allow identification of those who are at increased risk of dying from pneumonia. This method will assess disease severity and monitor treatment progress.
Extending the Capabilities of Mobile Device Based Pulse Oximetry
With funding from NSERC, we have partnered with LionsGate Technologies Inc., a Canadian company and UBC spin-off, (LGTmedical; lgtmedical.com), to develop original smartphone-based sensors and mHealth software applications. Our team created the Phone Oximeter™, a series of mobile applications that incorporate a proprietary analog-to-digital AC-coupled bridging framework, the Vital Signs DSP™, to enable measurement of blood O2 saturation and heart rate. External hardware is minimal and the applications use inexpensive medical sensors that connect to devices through the universally-available audio port. Via such technical innovations, and by leveraging the ubiquity of devices and data networks in the developing world, the Phone Oximeter™ will radically reduce the cost of disease diagnosis and make monitoring of vital signs accessible worldwide. In this project, our research and development objectives are to improve the signal quality and extend the functional capabilities of the Vital Signs DSP™-driven Phone Oximeter™, including developing a sensor for neonates and infants.
Community Level Interventions for Pre-eclampsia
The hypertensive disorders of pregnancy (HDP), including pre-eclampsia, remain one of the top three categories of maternal mortality and morbidity, globally. The majority of deaths due to HDP occur in low and middle income countries. The Community Level Interventions for Pre-eclampsia (CLIP) trial is a large cluster randomised controlled trial happening in Mozambique, Pakistan and India using mobile applications developed by our group. Community healthcare workers use the CLIP PIERS on the Move mobile application to regularly assess pregnant women in their homes. The app uses the mini-PIERS (Pre-eclampsia Integrated Estimate of RiSk) predictive model to determine the probability of an adverse event in the next 48 hours and then provide a recommendation of regular care or antihypertensives and transport to a hospital.
Monitoring at Home Before and After Adenotonsillectomy
Tonsillectomy and/or adenoidectomy are commonly performed procedures in children. Occasionally some children can develop breathing problems after the operation. We are trying to use a new device to make tonsil and/or adenoid removal surgery as safe as possible. The device uses a pulse oximeter sensor connected to a mobile phone or tablet that records the levels of oxygen overnight. Families will use the device for three nights before and after tonsil and/or adenoid removal surgery in order to look at the changes that happen and see if we can predict which children could develop breathing problems after the operation.
Screen-My-Sleep: Validation of the Phone Oximeter as an At‐home Sleep Apnea Screening Tool for Children
The diagnosis of sleep apnea in children and youth presents a challenging problem. Polysomnography (PSG) is the standard test for the diagnosis of sleep apnea. This test requires a comprehensive sleep laboratory and the inconvenience of an overnight stay. We are trying to use a new device to identify sleep apnea in children by using a pulse oximeter sensor connected to a mobile phone or tablet that records the levels of oxygen overnight. We are using the device at the same time as the hospital sleep study, and then again for two nights at home.
VitalPAD: an intelligent monitoring and communication device to optimize safety in the pediatric intensive care unit (PICU)
The goal was to develop a unified, portable and intelligent device that integrated information from multiple patient monitors, mechanical ventilators, infusion pumps and clinical information systems. It allowed PICU healthcare team members, on or off-site, to monitor critically ill patients continuously. The project involved two components: a) We used feedback obtained in a participatory design process to guide the development of the VitalPAD, and b) We used simulated ICU scenarios, to evaluate whether clinicians would prioritize the care of critically ill patients more rapidly and more accurately with the use of VitalPAD than without it.
Testing of a novel pulse oximeter clip
The purpose of this study is to gather data from a novel pulse oximeter clip, which combines an optical and a mechanical measurement method. Traditionally, pulse oximetry obtains oxygen saturation and the plethysmographic waveform through a light absorption method. However, similar data could also be obtained by recording a change in the finger diameter, triggered by the pressure wave of arterial blood in the finger, using a piezoelectric sensor. This mechanical sensor might be a good alternative and/or addition to the common pulse oximeter. The advantages of the mechanical sensor is that provides insight into the pressure/volume relationships of blood flow in the finger required less power than a pulse oximeter so could be used for extracting heart rate in low power applications.
Development of predictive analytics for impending cardiac arrest in children admitted to the Pediatric Intensive Care Unit
Assignment of priority of care and early detection of deterioration of critically ill patients in the Intensive Care Unit (ICU) represent an enormous source of preventable morbidity, mortality and cost. In comparison to adults, children have smaller functional reserves and deteriorate faster when critically ill. The task of preventing/predicting adverse events, such as cardiac arrests, is of paramount importance in improving patient safety in the PICU. Outcomes after cardiac arrest, including arrests witnessed in-facility, remain poor. Hence early detection of deterioration before the arrest is very important. The aim of this project was to develop predictive algorithms to predict adverse events in the PICU.
Respiratory Rate Counter – The RRate app
Respiratory rate (RR) is a fundamental measurement for disease diagnosis, prognosis, and treatment in children. Unfortunately, many studies have demonstrated that clinically obtained measures can be inaccurate in a variety of health-care settings. We have developed and validated a mobile phone application for the efficient and accurate measurement of respiratory rate. The RRate app is available for Android and iOS, and can also be used directly in a browser at rrate.netlify.app.
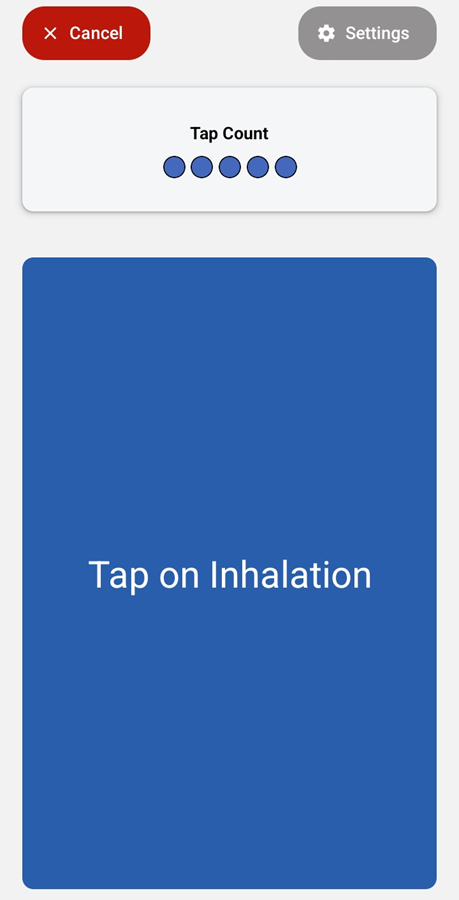
The touch screen is tapped each time the child inhales.
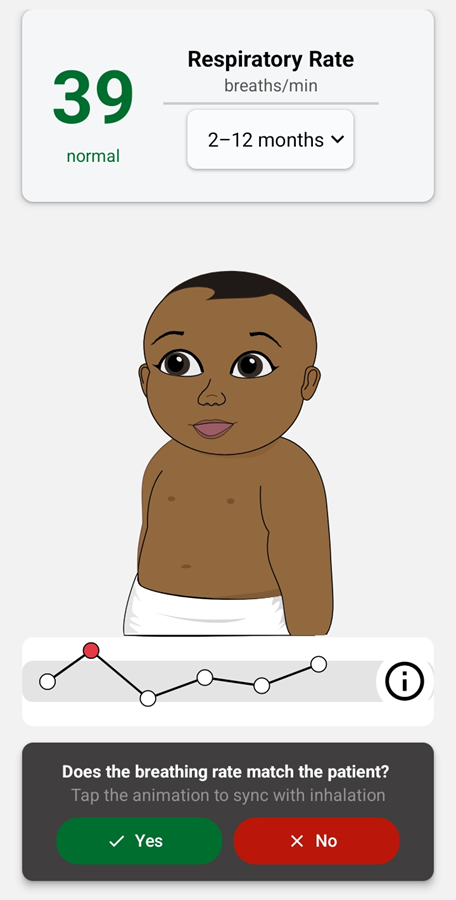
Once enough consistent taps have been made an animation of a baby breathing is displayed.
Detecting Fast Breathing
One of the keys to detecting pneumonia in children, is the measurement of Respiratory Rate, specifically determining if a child has fast breathing. The World Health Organization’s (WHO) Integrated Management of Childhood Illness guidelines identify fast breathing as 50 breaths per minute or more in children aged 2 months to 12 months and 40 breaths per minute or more in children aged 12 months up to 5 years. As seen above, the RRate app can display whether the respiratory rate is normal or high once you enter an age category for the child.
The WHO promotes measuring RR by counting the number of breaths in a minute. There are many limitations to this method. It is time consuming and requires full attention. If any disruption to the counting occurs, the minute must be restarted. The RRate application is meant to solve this problem by providing a mobile application that can accurately calculate the respiratory rate in less than 10 seconds.
Detecting Consistent Taps
The RRate app displays the RR value as soon as enough consistently timed taps have been performed. Two parameters control this consistency check, as shown on the Configuration settings page of the application. This is only accessibly with a password, since the app defaults to the settings recommended by our research studies.
The first parameter, z, is the number of taps used in the RR calculation. If z = 4, then the RR is calculated based on the median of the 3 time intervals between the most recent 4 taps. This means you must tap at least 4 times, and if the 4 taps are not consistent enough, then you keep tapping and each time you tap the consistency is checked again using the timing of the most recent 4 taps. In the app, z is set to 5 by default.
The second parameter, C, is the consistency threshold necessary for the time intervals between the most recent z taps. The consistency zone is defined as the median of these intervals plus and minus C% of this median. For example, if the median time interval = 2.0 seconds and C = 10%, the time intervals must all be in the range of 1.8 – 2.2 seconds. If they are in this range the application shows a breathing baby with animation and sound/vibration for confirmation of the RR. If one or more of the time intervals is not in this range, the user must keep tapping. In the app, C is set to 13% by default.
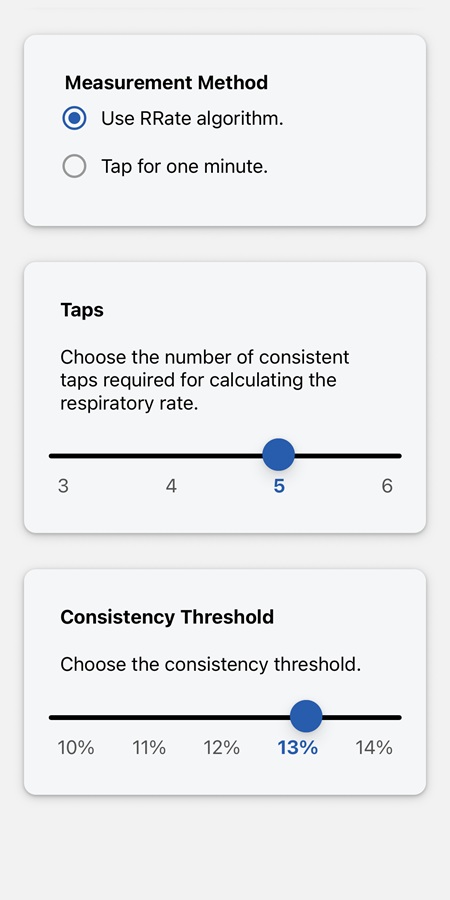
The number of taps and consistency threshold can be set on the setting configuration page if you have the password.
Publications
See our publications behind all the research done to choose the app default settings and test the app’s accuracy, efficiency, and repeatability in a real-world setting.
A Asdo, A Mawji, I Omara, IA Aye Ishebukara, C Komugisha, SK Novakowski, Y Pillay, MO Wiens, S Akech, F Oyella, A Tagoola, N Kissoon, JM Ansermino, D Dunsmuir. (2025) Repeatability of RRate measurements in children during triage in two Ugandan hospitals. PLOS Glob Public Health 5(1): e0003097. doi.org/10.1371/journal.pgph.0003097
Society for Technology in Anesthesia 2014 Annual Meeting abstract which won the Best Clinical Application award:
A Asdo, A Mawji, I Omara, C Agaba, C Komugisha, S Novakowski, Y Pillay, M Wiens, S Akech, F Oyella, A Tagoola, N Kissoon, JM Ansermino, D Dunsmuir. Repeatability of Respiratory Rate Measurements in Children during Triage in Two Ugandan Hospitals. Anesthesia & Analgesia 138(4S):p 1-104, April 2024. doi.org/10.1213/01.ane.0001011528.18574.c2
H Gan, W Karlen, D Dunsmuir, G Zhou, M Chiu, GA Dumont, JM Ansermino (2015) The Performance of a Mobile Phone Respiratory Rate Counter Compared to the WHO ARI Timer. J Healthc Eng, 6(4), 691-703. doi.org/10.1260/2040-2295.6.4.691
W Karlen, H Gan, M Chiu, D Dunsmuir, G Zhou, GA Dumont, & JM Ansermino (2014). Improving the Accuracy and Efficiency of Respiratory Rate Measurements in Children Using Mobile Devices. PLoS ONE, 9(6), e99266. doi.org/10.1371/journal.pone.0099266
Society for Technology in Anesthesia 2014 Annual Meeting abstract:
The Design of a Respiratory Rate Mobile Application
Code and Configuration
The RRate app code is available on a public GitHub repository for anyone to see and the Wiki on the GitHub repository explains how to configure it to upload to REDCap or for use with another application using the SMART on FHIR protocol.