What is Smart Triage?
 Smart Triage is a digital platform that enables the triage of sick and critically ill children at health facilities in low resourced settings. The platform consists of:
Smart Triage is a digital platform that enables the triage of sick and critically ill children at health facilities in low resourced settings. The platform consists of:
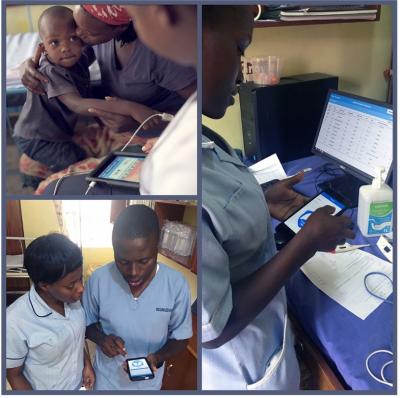
- Smart Triage mobile app: Using predictive algorithms this mobile application allows healthcare providers to triage pediatric patients efficiently and effectively. The triage process is supported by pulse oximetry and the integration of a custom pulse oximetry application. Once triaged, children are assigned a risk category which allows health care providers to easily identify emergency and high risk children to ensure they receive the lifesaving care they need as quickly as possible. The predictive algorithm was developed and is updated based on actual outcomes.
- Clinician dashboard: Linked to the mobile application this interactive dashboard is accessed through a laptop or tablet. It displays real time data on patient risk prioritization, demographics, time to treatment, and their location in the facility. The dashboard also includes customized reports that
 can be used by the hospital to track treatment times, set and monitor health care quality benchmarks and facilitate ongoing quality improvement.
can be used by the hospital to track treatment times, set and monitor health care quality benchmarks and facilitate ongoing quality improvement.
- Smart Spot: Integrated with the mobile application and clinician dashboard, this Bluetooth enabled treatment tracking and patient location system allows health care workers to easily identify priority and high risk patients and monitor treatment times to ensure the timely provision of care.
Together, the Smart Triage platform uses a data-driven approach to improve the quality of care for children suffering from severe infectious illness and enables the allocation of scarce resources more efficiently. The goal of Smart Triage is to enable healthcare workers to recognize children in need of emergency treatment more rapidly, deploy resources efficiently to enable timely care and improve pediatric outcomes.
Why is Smart Triage needed?
In low resource settings, patients are frequently admitted and treated on a first-come, first-serve basis, leading to delayed care for children who are in need of urgent treatment. Sepsis, defined as a systemic response to infection that leads to vital organ dysfunction, is a leading cause of death and disability in children. These children can receive faster treatment if every child is rapidly triaged upon arrival to identify danger and priority signs of sepsis. Sepsis however, is a syndrome that mimics many conditions and few health workers can confidently triage and diagnose sepsis. With Sepsis, every hour of delay in treatment is associated with greater risks of organ damage and death.

The purpose of Smart Triage is to develop and clinically evaluate a digital triage tool that can be used to rapidly and reliably, without the need for extensive memorization or training by frontline health workers, identify critically ill children (including those with sepsis) and get them the care they need as quickly as possible.
In addition to shortening time to treatment and improving health outcomes for critically ill children, the Smart Triage platform has been designed to support hospitals and health care teams with their healthcare quality improvement (QI) efforts. Due to a variety of factors, quality of care in many low resource settings is suboptimal and associated with more than 8 million deaths yearly from conditions that should be treatable by the health system. QI is a continuous day to day process of identifying areas for improvement and implementing solutions to address them. Smart Triage can contribute to QI efforts by providing critical high-quality data to strengthen leadership and governance, engage the workforce, and facilitate optimal use of resources.
How did we develop Smart Triage?
In 2017 the Institute for Global Health (IGH; formerly the Centre for International Child Health) at BC Children's Hospital and BC Women’s Hospital + Health Centre was awarded $250,000 as a finalist in the Google.org Impact Challenge. The innovation proposed was the Pocket Doc for Pneumonia, a low-cost smartphone tool that would help health care workers in remote areas and developing countries to accurately diagnose pneumonia and save children's lives. The project was deployed in Uganda in 2018, with partner health facility Holy Innocents Children's Hospital.
 In 2019, a grant was generously awarded by the Wellcome Trust, to engage in the next phase of this project — Smart Triage. This phase of the project aimed to validate the predictive algorithms used in the Paediatric Rapid Sepsis Trigger (PRST) tool, the basis of the Smart Triage risk prioritization model used in the Smart Triage app. The work on the this phase of the project began in September 2019 and was completed at two sites in Kenya and Uganda, with support from our partners at the Kenya Medical Research Institute (KEMRI) and Walimu in Uganda.
In 2019, a grant was generously awarded by the Wellcome Trust, to engage in the next phase of this project — Smart Triage. This phase of the project aimed to validate the predictive algorithms used in the Paediatric Rapid Sepsis Trigger (PRST) tool, the basis of the Smart Triage risk prioritization model used in the Smart Triage app. The work on the this phase of the project began in September 2019 and was completed at two sites in Kenya and Uganda, with support from our partners at the Kenya Medical Research Institute (KEMRI) and Walimu in Uganda.
In Uganda, baseline data collection for the PRST study began in May of 2020 at Jinja Regional Referral Hospital. The PRST model was validated using data collected from a total of 1756 participants and the validated model was integrated into the Smart Triage mobile application. User testing for the Smart Spot automated patient and treatment tracking system was completed, and the entire Smart Triage triaging platform (i.e., mobile application, clinician dashboard, and Smart Spot) was implemented at Jinja Regional Referral Hospital (JRRH) in April 2021.
In Kenya, baseline data collection to validate the PRST model began in February 2021 at Mbagathi County Hospital. The model was validated using data collected from 2856 participants and the Smart Triage triaging platform was implemented in December 2021. The model has since been integrated into the Dormax electronic medical record (EMR) platform currently at Mbagathi County Hospital, to support its continued use at the facility.
Implementation of Smart Triage+QI
In 2020, we partnered with Walimu and the Uganda Catholic Medical Bureau (UCMB) to expand the Smart Triage platform to an additional four hospitals in Uganda with the support of Grand Challenges Canada, funded by the Government of Canada. This funding provided an opportunity to develop a scalable package of training materials on data-driven quality improvement (i.e., Smart Triage+QI) which can be used by health workers, hospital leadership, and health decision-makers to integrate this improved approach to triaging at public and private facilities across Uganda.
In 2022, we implemented Smart Triage+QI at Gulu Regional Referral Hospital, St Joseph’s Hospital Kitovu, and Uganda Martyrs’ Ibanda Hospital, and supported Holy Innocents Children’s Hospital with transitioning from use of Pocket Doc for Pneumonia to Smart Triage+QI. We also partnered with Kisiizi Hospital in Uganda to integrate the PRST model into their Streamline EMR, which has supported use of the Smart Triage approach at this facility. As of November 2024, over 150,000 children have been triaged using the Smart Triage platform, and over 350 health workers have been trained in use of Smart Triage and QI.
Publications
-
Huxford C, Hwang B, Dunsmuir D, Pillay Y, Tusingwire F, Oyella FO, Akello B, Aye Ishebukara IA, Novakowski SK, Opar BT, Kenya-Mugisha N, Tagoola A, Wiens MO, Kissoon N, Ansermino JM. Exploring two-way text messages for post-discharge follow-up and quality improvement in rural Uganda. PLoS One. 2025 Aug 11;20(8): e0322969. doi: 10.1371/journal.pone.0322969
-
Goertzen R, Pillay Y, Karugaba J, Aye Ishebukara IA, Asdo A, Dunsmuir D, Behan J, Huxford C, Novakowski SK, Tusingwire F, Kasyaba R, Kakuru G, Khisa J, Businge S, Kyewalyanga M, Kissoon N, Ansermino JM. Improving pediatric care in Uganda with a digital platform and quality improvement initiative: A retrospective review of Smart Triage + QI. PLoS One. 2025 Aug 7;20(8): e0329369. doi: 10.13
-
Asdo A, Mawji A, Omara I, Aye Ishebukara IA, Komugisha C, Novakowski SK, Pillay Y, Wiens MO, Akech S, Oyella F, Tagoola A, Kissoon N, Ansermino JM, Dunsmuir D. Repeatability of RRate measurements in children during triage in two Ugandan hospitals. PLOS Glob Public Health. 2025 Jan 7;5(1):e0003097. doi: 10.1371/journal.pgph.0003097. PMID: 39775211; PMCID: PMC11706398.
-
Ansermino JM, Pillay Y, Tagoola A, Zhang C, Dunsmuir D, Kamau S, Kigo J, Agaba C, Aye IA, Hwang B, Novakowski SK, Huxford C, Wiens MO, Kimutai D, Ouma M, Ahmed I, Mwaniki P, Oyella F, Tenywa E, Nambuya H, Toliva BO, Kenya-Mugisha N, Kissoon N, Akech S; Pediatric Sepsis CoLab. Implementation of Smart Triage combined with a quality improvement program for children presenting to facilities in Kenya and Uganda: An interrupted time series analysis. PLOS Digit Health. 2025 Mar 10;4(3):e0000466. doi: 10.1371/journal.pdig.0000466. PMID: 40063663; PMCID: PMC11892856.
-
Kamau S, Kigo J, Mwaniki P, Dunsmuir D, Pillay Y, Zhang C, Nyamwaya B, Kimutai D, Ouma M, Mohammed I, Gachuhi K, Chege M, Thuranira L, Ansermino JM, Akech S. Comparison between the Smart Triage model and the Emergency Triage Assessment and Treatment guidelines in triaging children presenting to the emergency departments of two public hospitals in Kenya. PLOS Digit Health. 2024 Aug 1;3(8):e0000408. doi: 10.1371/journal.pdig.0000408.
-
Zhang C, Wiens MO, Dunsmuir D, Pillay Y, Huxford C, Kimutai D, Tenywa E, Ouma M, Kigo J, Kamau S, Chege M, Kenya-Mugisha N, Mwaka S, Dumont GA, Kissoon N, Akech S, Ansermino JM; Pediatric Sepsis CoLab. Geographical validation of the Smart Triage Model by age group. PLOS Digit Health. 2024 Jul 1;3(7):e0000311. doi: 10.1371/journal.pdig.0000311.
-
Kigo J, Kamau S, Mawji A, Mwaniki P, Dunsmuir D, Pillay Y, Zhang C, Pallot K, Ogero M, Kimutai D, Ouma M, Mohamed I, Chege M, Thuranira L, Kissoon N, Ansermino JM, Akech S. External validation of a paediatric Smart triage model for use in resource limited facilities. PLOS Digit Health. 2024 Jun 21;3(6):e0000293. doi: 10.1371/journal.pdig.0000293.
-
Li ECK, Tagoola A, Komugisha C, Nabweteme AM, Pillay Y, Ansermino JM, Khowaja AR. Cost-effectiveness analysis of Smart Triage, a data-driven pediatric sepsis triage platform in Eastern Uganda. BMC Health Serv Res. 2023 Aug 31;23(1):932. doi: 10.1186/s12913-023-09977-5.
-
Asdo A, Mawji A, Agaba C, Komugisha C, Novakowski SK, Pillay Y, Kamau S, Wiens MO, Akech S, Tagoola A, Kissoon N, Ansermino JM, Dunsmuir D. Repeatability of Pulse Oximetry Measurements in Children During Triage in 2 Ugandan Hospitals. Glob Health Sci Pract. 2023 Aug 28;11(4):e2200544. doi: 10.9745/GHSP-D-22-00544.
-
Mwaniki P, Kamanu T, Akech S, Dunsmuir D, Ansermino JM, Eijkemans MJC. Using self-supervised feature learning to improve the use of pulse oximeter signals to predict paediatric hospitalization. Wellcome Open Res. 2023 Feb 1;6:248. doi: 10.12688/wellcomeopenres.17148.2.
-
Mawji A, Longstaff H, Trawin J, Dunsmuir D, Komugisha C, Novakowski SK, Wiens MO, Akech S, Tagoola A, Kissoon N, Ansermino JM. A proposed de-identification framework for a cohort of children presenting at a health facility in Uganda. PLOS Digit Health. 2022 Aug 24;1(8):e0000027. doi: 10.1371/journal.pdig.0000027.
-
Mawji A, Li E, Dunsmuir D, Komugisha C, Novakowski SK, Wiens MO, Vesuvius TA, Kissoon N, Ansermino JM. Smart triage: Development of a rapid pediatric triage algorithm for use in low-and-middle income countries. Front Pediatr. 2022 Nov 22;10:976870. doi: 10.3389/fped.2022.976870.
- Novakowski SK, Kabajaasi O, Kinshella, MLW, Pillay Y, Johnson T, Dunsmuir D, Pallot K, Rigg J, Kenya-Mugisha N, Opar B, Ansermino JM, Tagoola A, Kissoon N. Health worker perspectives of Smart Triage, a digital triaging platform for quality improvement at a referral hospital in Uganda: a qualitative analysis. BMC Pediatrics; 22:593. doi: 10.1186/s12887-022-03627-1
- Mawji A, Akech S, Mwaniki P, Dunsmuir D, Bone J, Wiens MO, Gorges M, Kimutai D, Kissoon N, English M, Ansermino JM. Derivation and internal validation of a data-driven prediction model to guide frontline health workers in triaging children under-five in Nairobi, Kenya [version 3; peer review: 2 approved]. Wellcome Open Research 2021; 4:121
- Mawji A, Li E, Chandna A, Kortz T, Akech S, Wiens MO, Kissoon N, Ansermino JM. Common data elements for predictors of pediatric sepsis: A framework to standardize data collection. PLOS ONE 2021; 16(6):e0253051.
- Mawji A, Li E, Komugisha C, Akech S, Dunsmuir D, Wiens MO, Kissoon N, Kenya-Mugisha N, Tagoola A, Kimutai D, Bone J, Dumont G, Ansermino JM. Smart triage: triage and management of sepsis in children using the point-of-care Pediatric Rapid Sepsis Trigger (PRST) tool. BMC Health Services Research 2020; 20:493.
- Lee V, Dunsmuir D, Businge S, Tumusiime R, Karugaba J, Wiens MO, Gorges M, Kissoon N, Orach S, Kasyaba R, Ansermino JM. Evaluation of a digital triage platform in Uganda: A quality improvement initiative to reduce the time to antibiotic administration. PLOS ONE 2020; 15(10): e0240092.
- Zhou G, Karlen W, Brant R, Wiens MO, Kissoon N, Ansermino JM. A transformation of oxygen saturation (the saturation virtual shunt) to improve clinical prediction model calibration and interpretation. Pediatric Research 2019; 86(6):732-737.
- Fung JST, Akech S, Kissoon N, Wiens MO, English M, Ansermino JM. Determining predictors of sepsis at triage among children under 5 years of age in resource-limited settings: A modified Delphi process. PLOS ONE 2019; 14(1): e0211274.
- Lavoie PM, Popescu CR, Molyneux EM, Wynn JL, Chiume M, Keitel K, Lufesi N, Levine GA, Ansermino JM, Kissoon N. Rethinking management of neonates at risk of sepsis. The Lancet 2019; 394(10195):279-281.
- Liang LD, Kotadia N, English L, Kissoon N, Ansermino JM, Kabakyenga J, Lavoie PM, Wiens MO. Predictors of Mortality in Neonates and Infants Hospitalized With Sepsis or Serious Infections in Developing Countries: A Systematic Review. Frontiers in Pediatrics 2018; 6:277.
- Garde A, Zhou G, Raihana S, Dunsmuir D, Karlen W, Dekhordi P, Huda T, Arifeen SE, Larson C, Kissoon N, Dumont G, Ansermino JM. Respiratory rate and pulse oximetry derived information as predictors of hospital admission in young children in Bangladesh: a prospective observational study. BMJ Open 2016; 6:e011094.
- Wiens MO, Larson C, Kumbakumba E, Kissoon N, Ansermino JM, Singer J, Wong H, Ndamira A, Kabakyenga J, Moschovis P, Kiwanuka J. Application of Sepsis Definitions to Pediatric Patients Admitted With Suspected Infections in Uganda. Pediatric Critical Care Medicine 2016; 17(5):400-405.
- Lowlaavar N, Larson CP, Kumbakumba E, Zhou G, Ansermino JM, Singer J, Kissoon N, Wong H, Ndamira A, Kabakyenga J, Kiwanuka J, Wiens MO. Pediatric in-Hospital Death from Infectious Disease in Uganda: Derivation of Clinical Prediction Models. PLOS ONE 2016; 11(3): e0150683.
- Karlen W, Dunsmuir D, Ansermino JM. Efficiency of respiratory rate measurements: Comment on Black et al., 2015: “Can simple mobile phone applications provide reliable counts of respiratory rates in sick infants and children? An initial evaluation of three new applications”. International Journal of Nursing Studies 2015; 52(7):1279-1280.
- Gan H, Karlen W, Dunsmuir D, Zhou G, Chiu M, Dumont G, Ansermino JM. The Performance of a Mobile Phone Respiratory Rate Counter Compared to the WHO ARI Timer. Journal of Healthcare Engineering 2015; 6.
- Raihana S, Dunsmuir D, Huda T, Zhou G, Rahman QSu, Garde A, Moinuddin M, Karlen W, Dumont G, Kissoon N, Arifeen SE, Larson C, Ansermino JM. Development and Internal Validation of a Predictive Model Including Pulse Oximetry for Hospitalization of Under-Five Children in Bangladesh. PLOS ONE 2015;10(11): e0143213.
- Karlen W, Gan H, Chiu M, Dunsmuir D, Zhou G, Dumont G, Ansermino JM. Improving the Accuracy and Efficiency of Respiratory Rate Measurements in Children Using Mobile Devices. PLOS ONE 2014; 9(6): e99266.
- Karlen W, Wiens M.O, Gan H, Dunsmuir D, Chiu M, Dumont G, Ansermino JM. Assessing the Quality of Manual Respiratory Rate Measurements using Mobile Devices. IET Conference Publications 2014; 1-4.
- Peterson CL, Chen TP, Ansermino JM, Dumont G. Design and Evaluation of a Low-Cost Smartphone Pulse Oximeter. Sensors 2013; 13(12):16882-16893.
Our Team
The Smart Triage team includes experts with strengths and perspectives from different fields, countries, and contexts. The Institute for Global Health (IGH; formally the Centre for International Child Health) at BC Children's Hospital and BC Women’s Hospital + Health Centre coordinates activities for the team. Our team includes experts in child health, sepsis, neonatology, mobile health, epidemiology, technology, engineering, software development, business, and program management.
Research Team
- Dr. Samuel Akech – Principal Investigator, KEMRI-Wellcome Trust Research Programme
- Dr. Nathan Kenya Mugisha – Executive Director, Walimu
- Dr. Abner Tagoola – Head of Department Paediatrics, Jinja Regional Referral Hospital
- Dr. Sam Orach – Executive Secretary, Uganda Catholic Medical Bureau
- Dr. Ronald Kasyaba – Assistant Executive Secretary, Uganda Catholic Medical Bureau
- Dr. Yashodani Pillay – Postdoctoral Research Fellow, UBC, Department of Anesthesiology, Pharmacology and Therapeutics; Project Coordinator, IGH
- Dr. Mark Ansermino – Executive Medical Director, Global Health; Co-Director, Digital Health Innovation Lab at BC Children’s; Professor, UBC Department of Anesthesia, Pharmacology and Therapeutics
- Dr. Niranjan Kissoon – Professor, UBC Departments of Pediatrics and Surgery (Emergency Medicine)
- Dr. Matthew O. Wiens – Investigator, IGH; Assistant Professor, UBC Department of Anesthesia, Pharmacology and Therapeutics
- Dr. Guy Dumont – Investigator, BC Children’s Hospital; Co-Director, Digital Health Innovation Lab at BC Children’s; Professor, UBC Department of Electrical and Computer Engineering
- Dr. David Kimutai – Paediatrician, Mbagathi County Hospital Kenya
- Dr. Paska Apiyo – Deputy Director, Gulu Regional Referral Hospital, Uganda
- Dr. Florence Oyella – Head of Department Paediatrics, Gulu Regional Referral Hospital
- Dr. Benard Opar – Technical Coordinator, Walimu, Uganda
- Fredson Tusingwire – Project Coordinator, Walimu
- Savio Mwaka – Program Manager, Walimu
- Catherine Kiggundu – Accountant, Walimu
- Dr. Stephen Businge – Holy Innocents Children’s Hospital, Uganda
- James Karugaba – Holy Innocents Children’s Hospital
- Ivan Aine Aye Ishebukara – Information Technology Specialist, Holy Innocents Children’s Hospital, and Walimu
- Mike English – Head of the Clinical Information Network (CIN), KEMRI-Wellcome Trust Research Programme
- Paul Mwaniki – Data Management, KEMRI-Wellcome Trust Research Programme
- Morris Ogero – Data Management, KEMRI-Wellcome Trust Research Programme
- Cynthia Khazenzi – Data Management, KEMRI-Wellcome Trust Research Programme
- Stephen Kamau – Study Coordination, KEMRI-Wellcome Trust Research Programme
- Joyce Kigo – Data Management, KEMRI-Wellcome Trust Research Programme
- Dr. Edmond Li – UBC, Department of Anesthesiology, Pharmacology and Therapeutics.
- Bella Hwang – Program Manager, IGH
- Dustin Dunsmuir – Technical Lead, IGH
- Charly Huxford – Research Assistant, IGH
- Stefanie Novakowski – Strategic Lead, Global Health Research Development, IGH
Support and Acknowledgements
The Smart Triage team gratefully acknowledges our implementing partners Walimu, KEMRI, and the Uganda Catholic Medical Bureau, as well as our funding partners, including Google, Wellcome Trust, Grand Challenges Canada, Mining4Life and the BC Children’s Hospital Foundation.

Contact
For more information, please contact Yash Pillay.